Last updated on: Oct 8th, 2020
Renal disease
- Most common causes: DM and HTN, control blood glucose and blood pressure can prevent renal damage.
- Dehydration is presented with BUN:SCr > 20:1, with symptoms: ↓ urine output, dry membrane, tachycardia.
- Creatinine: a waste product from muscle metabolism. As kidney function declines, Cr ↑. (Normal: 0.6-1.3 mg/dL)
- Albumin: primary protein used to assess kidney disease. (Albuminuria = proteinuria)
- Chronic kidney disease (CKD): GFR < 60 mL/min and/or albuminuria (>=30) Drug induced: Aminoglycosides, amphotericin B, polymyxins, vancomycin, cyclosporine/tacrolimus, loop diuretics, NSAIDs (including COX2, vasoconstriction in renal vessels), platinum-based chemo (cisplatin), radiographic contrast dye.
- Dosing adjustment is generally based on Cockcroft-Gault formula (see calculation chapter). A few drugs use GFR (SGLT2 inhibitors, and metformin).
- ACE or ARB: 1st line in CKD with albuminuria, diabetes, hypertension. (Inhibit RAA, causing efferent arteriolar dilation, reduce pressure in glomerulus, decrease albuminuria and provide CV protection).
- Thiazide diuretic: 1st line in CKD without albuminuria.
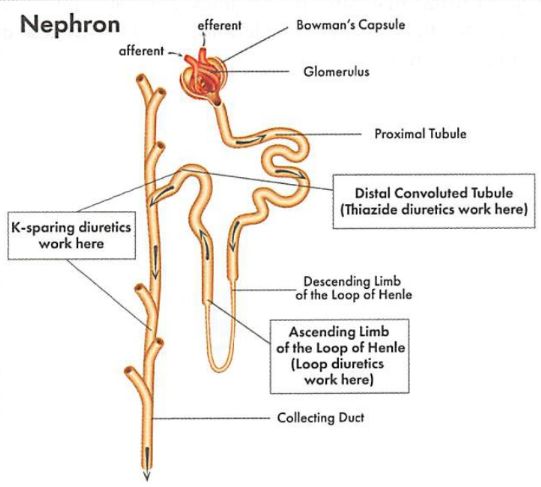
Loop of Henle
- Belongs to proximal convoluted tubule (PCT) and is located in medulla (inner part of kidney), loop of Henle creates osmotic gradient).
- PCT is the major reabsorption site.
- Descending limb: water reabsorption (permeable to water, but not solute).
- Ascending limb: salt reabsorption (permeable to salt, but not water).
- Loop diuretic: inhibits Na-K pump in the ascending loop of Henle, less Na is reabsorbed to the blood, and causes less Ca reabsorbed leading to Ca depletion. Long-term use may lead to decreased bone density.
Distal convoluted tubule (DCT)
- Located in cortex (outer shell of kidney) which contains the distal convoluted tubules (Distal means further away), fine tune the work done by proximal tubule for more reabsorption of salts and water.
- DCT is hormone controlled (aldosterone = ↑Na, ↓K, PTH=↑Ca).
- Thiazide diuretics: inhibit Na-Cl pump, since only 5% of Na is reabsorbed in this part, thiazide is a weaker diuretic than loops; thiazides ↑ Ca reabsorption leading to protective effect on bones.
- Aldosterone antagonists (spironolactone, eplerenone): ↓ Na and water through excretion in the urine, and ↑ serum K.
Collecting duct
- Connects the nephron to the ureter, and is involved in water and electrolytes balance, which is affected by ADH and aldosterone.
- Aldosterone: works in distal convoluted tubule and collecting duct to increase Na and water reabsorption and decrease K reabsorption.
- Aldosterone antagonists (spironolactone, eplerenone): more Na and water are excreted in the urine and serum K increase.
Renal Dose Adjustment
- Basic principle: primary concerns are drugs eliminated through the kidney and the accumulation can lead to toxicity. The dose or dosing interval is reduced.
- Refer to the chapter “Foundation” -> “Drug interaction/side effects” for more details on how to comprehend the list.
- CrCl < 60ml/min: renal dose adjustment; <30 ml/min contraindication.
Complications of CKD
- More frequent monitoring of parathyroid hormone (PTH), phosphate, Ca, K and V-D levels.
- PO4 levels increase because the kidney can not eliminate excess PO4 absorbed from diet.
- Kidney can not activate vitamin D, leading to decreased Ca absorption. Both high PO4 and low Ca stimulate release of PTH. In an individual with healthy kidneys, PTH causes increased Ca reabsorption, but in CKD, Ca would have been pulled from bones, leading to facture and demineralization.
- Chronically high level of phosphate continues to stimulate PTH release, causing hyper-Ca, leading to calcification and cardiovascular problems.
- Less erythropoietin (EPO) is produced by kidney, resulting in decreased RBC production and anemia.
Hyperphosphatemia
- Can elevate PTH, causes secondary hyperparathyroidism.
- Treatment: avoid dietary phosphate (dairy, cola, chocolate, nuts), and use phosphate binders.
- 3 types of Binders
- Aluminum based (Al hydroxide); SE: Al toxicity, constipation.
- Calcium based: calcium acetate (PhosLo), calcium carbonate (Tums); SE: hyper-Ca
- Aluminum and Ca free agents: sevelamer (Renvela, Renagel) can also lower cholesterol; iron based (ferric citrate, sucroferric) .
- Binder drug interactions: separate from levothyroxine and antibiotics that chelate (TCN and quinolones).
Vitamin D & secondary hyper-PTH
- High level of PTH is treated with vitamin D.
- Vitamin D deficiency occurs because it can not be activated by kidney to its active form: 1,23-dihydroxy vitamin D.
- 2 forms of D: D3 (cholecalciferol) is synthesized in skin after UV light exposure (sun), D2 (ergocalciferol) is produced from plant and is the primary dietary source of D.
- Vitamin D analog: increases Ca absorption and inhibits PTH. Calcitrol (rocaltrol) is an active form of D3.
- Calcimimetic: Increasing sensitivity of Ca receptors on parathyroid gland; cinacalcet (Sensipar) mimics action of Ca and causes reduction in PTH.
Anemia
- Erythropoiesis stimulating agent (ESA) can prevent the need for blood transfusion, however it can shorten survival and increase tumor progression. (prescriber no longer need to enroll ESA APPRISE oncology program since 2017 FDA feel they are adequately informed). ESAs are never used prophylactically, only for palliative care, not for cure.
- Anemia hgb < 13 g/dL; Only initiate ESA in Hgb <10, stop around 10 or 11.
- Takes 2-6 wks to work, don’t expect it to work overnight
- SE: HTN, stroke, thrombosis VTE, arrhythmia, CV death
- Drugs: Epoetin alfa (Procrit, Epogen), Darbepoetin (Aranesp)
Hyperkalemia
- Level > 5mEq/L, K is the most abundant intracellular cation.
- Lower level of K by: aldosterone hormone, diuretics (loops > thiazides)
- High level of K by: ACEI/ARB/aliskaren, K sparing agents (aldosterone antagonist), drosperinoneS-containing COC, transplant drugs (cyclosporin, tacrolimus), decreased renal excretion, diabetes (insulin insensitivity leads to reduced ability to shift K intracellularly)
- Treatment
- Shift K intracellularly: insulin, dextrose, sodium bicarb, albuterol
- Eliminate K from body: loops, sodium polystyrene sulfonate (Kayaxelate), hemodialysis.
Metabolic acidosis
- As the kidney function declines, the ability to absorb bicarbonate declines.
- Treatment in bicarb < 22: sodium bicarb. Monitor Na level as it can cause fluid retention.
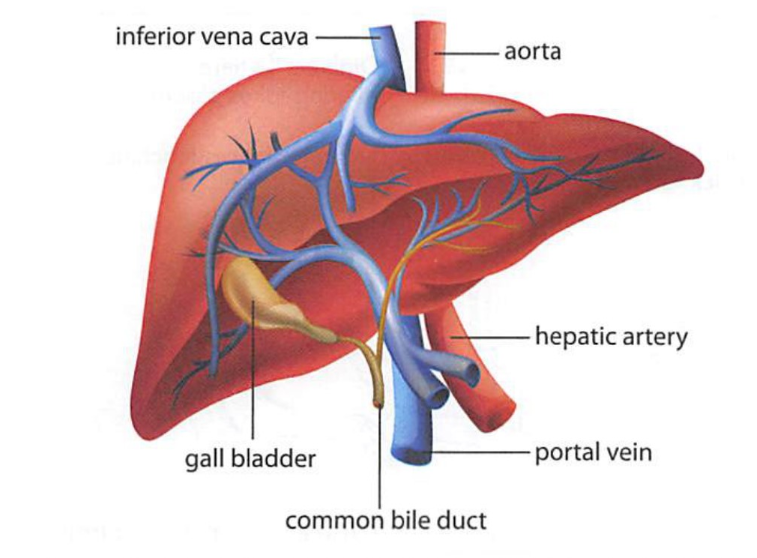
Liver diseases
Signs symptoms:
- Nausea/V/D, loss of appetite, malaise, abdominal pain in upper right quadrant, yellowed skin (jaundice), dark urine, pale stool.
- Labs: increased ALT/AST, decreased albumin (protein produced by liver), increased alkaline phosphatase, increased total bilirubin, increased PT.
Drugs with warning for hepatic damage
- TB meds (Rifampin, isoniazid)
- APAP overdose
- Antifungal drugs (ketoconazole, terbinafine)
- Anticonvulsants (phenytoin, phenobarbital, valproic acid)
- Rheumatoid arthritis drugs: such as infliximab (Remicade), MTX, chloroquine, hydroxychloroquine.
- Nefazodone
- Propylthiouracil (PTU)
- Tipranavir (TPV – a protease inhibitor)
- NRTIs
- Nevirapine
Hep-A
- Common and least severity.
- Transmission through contact of fecal, contaminated food.
- Vaccine: Havrix, Vaqta given to children starting age 1, or to older person with renal failure.
Hep-B & C
- Can cause acute illness and lead to chronic infection, cirrhosis, liver cancer and liver failure.
- Transmission through blood, or bodily fluid.
- Vaccine (Engerix-B, Recombivax H, Twinrix- 4 dose): 3 doses; no vaccine for C prevention.
- Milk thistle: a natural product derived from daisy, may have antioxidant and anti-inflammatory property that thought to help with liver diseases.
Hepatitis B
- NRTIs can be used as monotherapy, prior to starting, all patients should be tested for HIV.
- Boxed warning: lactic acidosis, hepatomegaly with steatosis, exacerbation of HBV
Hepatitis C
- Treatment approach is similar to HIV.
- Direct acting antivirals (DAAs): protease inhibitors (-previr, take with food), replication complex inhibitors (-asvir), and polymerase inhibitors (-buvir)
- SE: risk of reactivating hepatitis, increased LFTs.
- Preferred regimen contains 2-3 DAAs with different mechanisms.
- Drugs: sofosbuvir/ledipasvier (Harvoni), sofosbuvir/velpatasvir (Epclusa), Vosevi etc.
- Many drug interactions, many are CYP substrates: antiacid/H2RA/PPI can decrease concentration of sofosbuvir.
Interferon alfa
- Non-pegylated and pegylated (polyethylene glycol added, enhances half-life and reduces dosing frequency) for treatment of hepatitis B and C.
- Should not be injected IV, SC only
- BBW: autoimmune disorder, psychiatric symptoms, ischemic disease, infection.
Cirrhosis
- Advanced fibrosis (scarring) of liver, irreversible.
- Most common cause: hepatitis C, alcohol consumption.
Alcoholic liver disease
- BZD for alcohol withdrawal in inpatient; Anticonvulsants for outpatient
- Prevent relapse: naltrexone, disulfiram
- Thiamine (B1) treats Wernicke-Korsakoff disease (brain damage).
Nonalcoholic Fatty Liver Disease
- Usually without symptoms
- Goes hand in hand with obesity, high cholesterol, insulin resistance, and diabetes
- Mild form: fat buildup
- Severe form: can develop Inflammation, scarring (fibrosis), nonalcoholic steatohepatitis (NASH)
- Cornerstone of treatment: lifestyle modification
- Suggest pioglitazone for NASH patients, with or without diabetes (seems to reduce liver fat, inflammation, and tissue scarring); Caution about edema, weight gain, heart failure.
Portal hypertension
- Increased BP in hepatic portal vein, can cause variceal bleeding (enlarged vein in the lower part of esophageal). Medication that constricts circulation can minimize bleeding (octreotide is selective, vasopressin is non-selective)
- Non-selective beta blockers reduce portal pressure, and is added after resolution of bleeding to prevent reoccurrence. (It makes sense to use a non-selective instead of a selective BB which only works mostly in the heart)
Hepatic encephalopathy
- Caused by hepatic insufficiency.
- Symptoms: musty odor of breath, confusion, hand tremor, sluggish movements, resulted from nitrogenous substance in the blood (ammonia etc.)
- First line: non-absorbable disaccharides (lactulose) and antibiotics (rifaximin, neomycin)
- Lactulose works by converting ammonia (NH3) to ammonium (NH4+) (structure change from non-polar to polar, now can travel in blood to be excreted to urine) by gut bacteria.
- Antibiotics inhibit urease-producing bacteria, which decrease ammonia production.
- Zn serves as a cofactor in urea cycle and decrease ammonia concentration, avoid Zn deficiency.
Was this page helpful?
Back to top »