Last updated on: June 7th, 2019
Ischemic heart diseases
Background
- Angina: Chest pain, pressure, tightness, discomfort due to that heart muscle is not getting enough blood (ischemia of heart muscle or spasm of coronary arteries).
- Chest pain occur due to myocardial oxygen supply does not meet demand, usually caused by stenosis (narrowing of blood vessel), plaque buildup (atherosclerosis) or rupture in coronary arteries. Ischemia damages myocardial structure. This is known as coronary artery disease (CAD): narrowing of arteries and reduced flow to heart.
Stable angina
- Predictable chest pain, by exertion, relieved by rest or nitroglycerin (NTG). Also called silent ischemic heart disease (SIHD).
Prinzmetal's Angina
- Vasospasm of coronary arteries; can occur at rest, often by illicit drug use. CCB preferred, vasodilation
Silent Ischemia
- Transient ischemic attack (TIA) without symptoms of chest pain
- ST elevation/depression during activity
Unstable Angina
- Acute; a medical emergency where the chest pain is increasing, and not relieved by rest of NTG.
Treatment
- Goal: Reduce the risk of an acute coronary syndrome (MI) and provide symptomatic relief.
- Drug treatment: anti-platelet (ASA, or clopidogrel), anti-anginal agents (decease myocardial oxygen demand and increase supply): beta blockers (or CCB or long-acting nitrates, or ranolazine)
Antiplatelet
ASA
- Binds irreversibly to COX 1 and 2, leading to ↓ prostaglandin and thromboxane (a vasoconstrictor and inducer of platelet aggregation).
- NSAIDs increase the level of Lithium and methotrexate
- Salicylate allergy, children and teenage should avoid due to risk of Reye’s syndrome.
Clopidogrel
- binds irreversibly to inhibits P2Y12 mediated platelet aggregation.
- Prodrug, convert by CYP 2C19 to active metabolite.
- SE: thrombotic thrombocytopenia purpura (TTP) is rare.
- DI: avoid some PPIs (reduce effects of clopidogrel)
Anti-anginal Therapy
Beta blocker (BB)
- MOA: inhibit catecholamine effects, reduce oxygen demand. lead to ↓ HR (negative chronotropic), ↓contraction force (negative inotropic).
- 1st line in angina; More useful in silent ischemia than nitrates, CCB
- Start low and titrate slow.
- Avoid in Prinzemetal angina.
Calcium channel blocker (CCB)
- MOA: targets Ca channel lead to vasodilation, all CCB increase blood flow through coronary arteries.
- Preferred agent for Prinzmetal’s, or when BB is contraindicated.
- Use longer acting, avoid short acting. NDHP might be more effective
Nitrates
- decrease cardiac O2 demand by reducing preload, dilates coronary arteries, improves collateral blood flow.
- Call 911 if no relief after 1 dose.
- Do not use in low BP and low HR (SBP <90, HR<50), you do not want to aggravate the condition to cause hypoTN and extremely low HR
- DI: avoid PDE5 inhibitors
Ranolazine (Ranexa)
- MOA: inhibits Na current, ↓ intracellular Ca, may lead to decreased O2
- BP/HR neutral.
- Major 3A4 substrate, avoid use with 3A4 inhibitor/inducer (limit the dose to 500mg BID)
- QT prolongation due to effect on Na-channel.
Acute coronary syndrome (ACS)
Background
- Plaque buildup in coronary arteries (coronary atherosclerosis) causes sudden reduced blood flow to the heart and imbalance of myocardial oxygen supply and demand. It is a medical emergency.
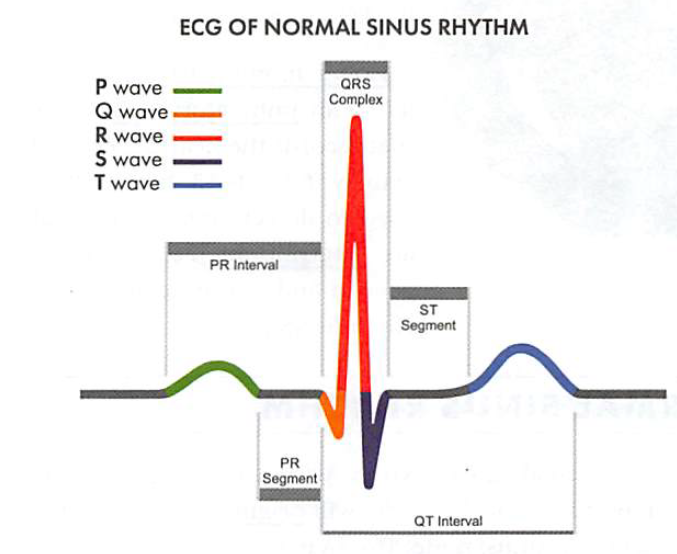
- ACS is an umbrella term containing a variety of symptoms. Patients with myocardial ischemia may or may not show ST elevation on ECG. ST elevation will eventually develop a Q-wave acute myocardial infarction (heart attack). Without ST elevation, patients either have unstable angina (UA) or non-ST elevation MI (NSTEMI). In a sentence, ST elevation is more acute and dangerous than non-ST elevation.
- Signs/symptoms: Severe radiating pain from sternum (to left shoulder, arm, jaw, back), Diaphoresis/SOB, N/V, tingling/numbness; can occur either at rest or exertion; Pain relieved by NTG at rest.
- Cardiac markers (troponin I and T) are detected after myocardial necrosis. The levels should be obtained for all patients with ACS.
Risk Factors
- Age: Men > 45, women > 55 or had hysterectomy
- Family history of coronary event: men > 55, women > 65.
- Smoking
- Existing cardiovascular diseases: Hyperlipidemia, HTN, DM.
Diagnosis
- NSTEMI: chest pain + cardiac enzymes (troponin T and I, or less sensitively CK-MB, CPK)
- STEMI: chest pain + cardiac enzymes + ST elevation (means needing more immediate reperfusion)
- UA (unstable angina): chest pain, no cardiac enzyme, no ECG changes
Standard care for ACS
- PCI: Coronary revisualization procedure, inflating a small balloon to widen coronary arteries to improve blood flow. Usually, a stent (metal mesh) is implanted in place to keep the artery open.
- MONA: give these immediately.
- GAP: give these next.
- BA: continue as outpatient.
Morphine
- Arteriolar/venous dilation, decrease myocardial O2 demand, pain reliever
- IV used in chest discomfort despite NTG. Usual dose 2-5mg IV PRN (FYI)
- Antidote: naloxone (Narcan)
Oxygen
- Used in cyanosis/respiratory distress, goal: >90% perfusion
Nitrates
- decrease cardiac O2 demand by reducing preload, dilates coronary arteries, improves collateral blood flow.
- Call 911 if no relief after 1 dose
- Do not use in low BP and low HR (SBP <90, HR<50), you do not want to aggravate the condition to cause hypoTN and extremely low HR
- DI: avoid PDE5 inhibitors
ASA
- Inhibits platelet aggregation and TXA2.
- chew 162-325mg non-enteric coated (take Plavix if intolerant)
2, + GAP
Glycoprotein (GP) IIb/IIIa receptor antagonist
- Agents: Abciximab (ReoPro), eptifibatide (Integrilin), tirofiban (Aggrastat)
- MOA: Block fibrinogen binding on platelets, prevent platelet aggregation and further thrombosis.
- CI: thrombocytopenia (Plt < 100,000), h/o bleeding diathesis and stroke, active internal bleeding, severe uncontrolled HTN, recent major surgery, renal dysfcn (eptifibatide, tirofiban), hypersensitivity to murine protein (abciximab)
- Used in PCI +/- stent intervention. Plt resumes function after d/c abciximab for 24 hrs, epti/tirofiban 4-8 hrs.
- SE: bleeding, TCP (esp. abciximab), GI (N), hypotension.
- All comes as injection, do not shake vial, must filter abciximab
Anti-coagulants
- Heparin, LMWH, bivalirudin
P2Y12 inhibitors
- clopidogrel (Plavix), Effient (prasugrel), ticargrelor (Brilinta)
- SE: bleeding, TTP (thrombotic thrombocytopenic purpura.
- Commonly used with ASA after ACS, known as dual antiplatelet therapy.
- Clopidogrel is a prodrug metabolized by CYP 2C19. (Check genotype before therapy initiation). Avoid strong 2C19 inhibitors (omeprazole, esomeprazole, other PPIs are less)
- DI: warfarin, SSRI and SNRI, NSAID increase risk of bleeding.
3. + BA, continue in outpatient.
BB:
· Decrease O2 demand by ↓ HR, BP and contractility.
- Low dose, B1 selective (without ISA activity) is preferred.
ACEI
- Prevents cardiac remodeling, ↓ preload & afterload
- oral therapy should be initiated in both LVHF & RVHF (as long as BP is ok), do not use IV w/in first 24 hr due to risk of hypoTN
+ fibrinolytics (optional)
- Drugs: alteplase (t-PA, Activase), tenecteplase (TNKase), reteplase (r-PA, Retevase)
- Binds to fibrin in a thrombus (clot), convert plasminogen to plasmin.
- PCI is preferred, but if PCI is not available, use fibrinolytic w/in 30 mins of arrival to the hospital, as an alternative. Used for STEMI only.
- SE: bleeding, hypotension, intracranial hemorrhage (due to HTN, important to keep low).
Long term management (second prevention after ACS)
- ASA 81 mg: indefinitely.
- P2Y12 inhibitor: at least 12 months, with or without ASA.
- NTG SL PRN: indefinitely.
- Beta blocker: if patient has HF.
- ACEI: indefinitely if EF <40%, DM, or CKD; consider for all MI patients.
- Aldosterone antagonist: indefinitely as an add-on if EF <40%, DM, or CKD.
- Statin: <75 y/o high intensity; > 75 y/o moderate-high intensity therapy.
Pain relief
- For pain relief, avoid NSAIDs, use APAP, ASA, tramadol, short term narcotic analgesics.
- If no other options, use a non-selective naproxen (lowest CV risk); avoid COX2 selective (high CV risk).
Anticoagulation
- If the patient has AFib, warfarin is needed. Triple combination (ASA, P2Y12 inhibitor, warfarin): shortest time possible, lower INR target (2-2.5).
- A dd a PPI for h/o of GI bleeding.
Quiz
Which of the following is a common side effect of nitroglycerin?
- Stevens-Johnson syndrome
- Arrhythmia
- Bleeding
- Headache
- Hypokalemia
Nitroglycerin is available in which of the following formulations? (Select ALL that apply)
- Patch
- Ointment
- SL tab
- Nasal spray
- Injection
Answers
- D. Nitroglycerin could potentially cause headaches. Nitroglycerin does not cause cardiac arrhythmias, bleeding, hypo or hyperkalemia, or Stevens-Johnson syndrome.
2. ABCE. Nitroglycerin is currently available as an intravenous injection, sublingual tab and spray, topical ointment, rectal ointment (for chronic anal fissures), and a transdermal patch. It is not available as a nasal spray.
Was this page helpful?
Back to top »