Updates: Feb 28th, 2021
March 13th, 2019
Background
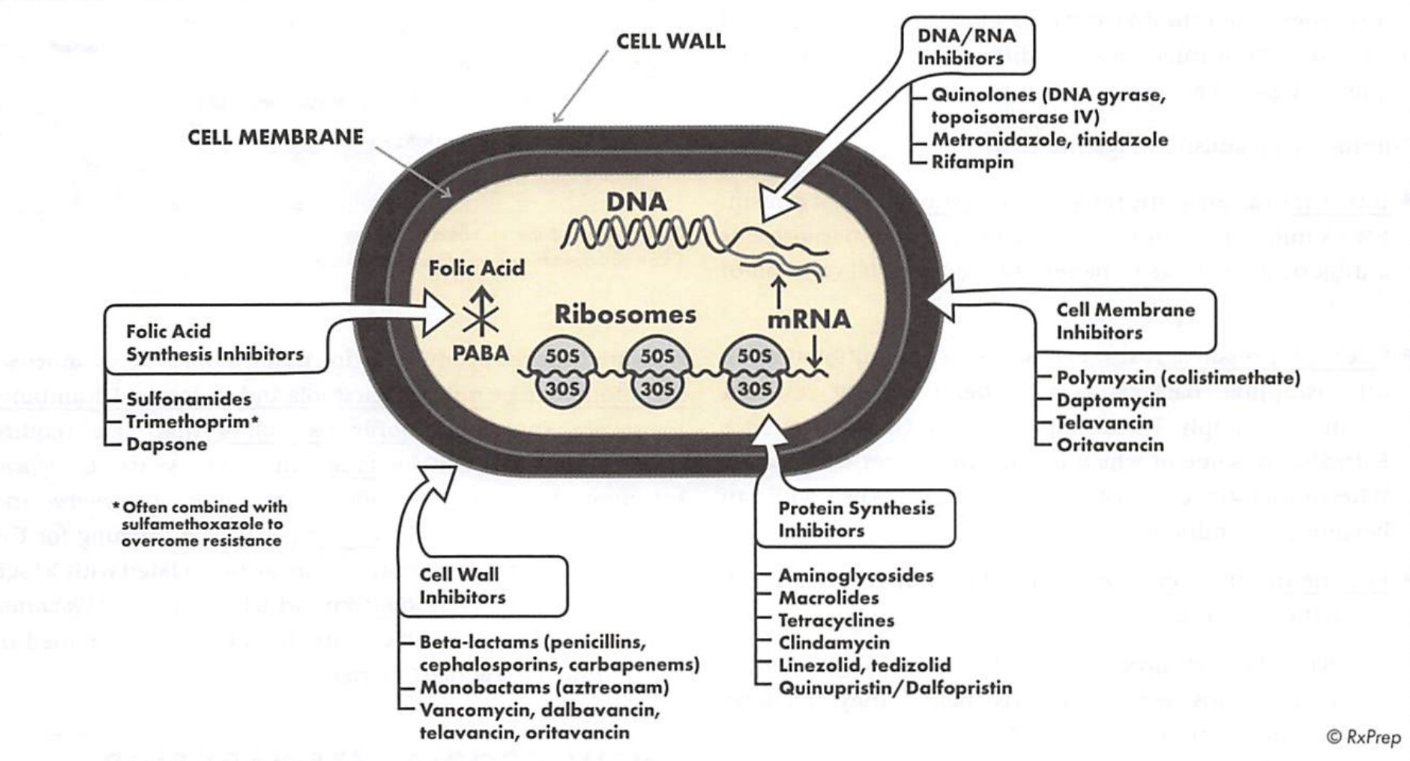
- Careful selection of an appropriate antibiotic agent is the paramount success in treating an infection. Both drug dose and interval are important considerations, in preventing treatment failure, drug resistance, and toxicities.
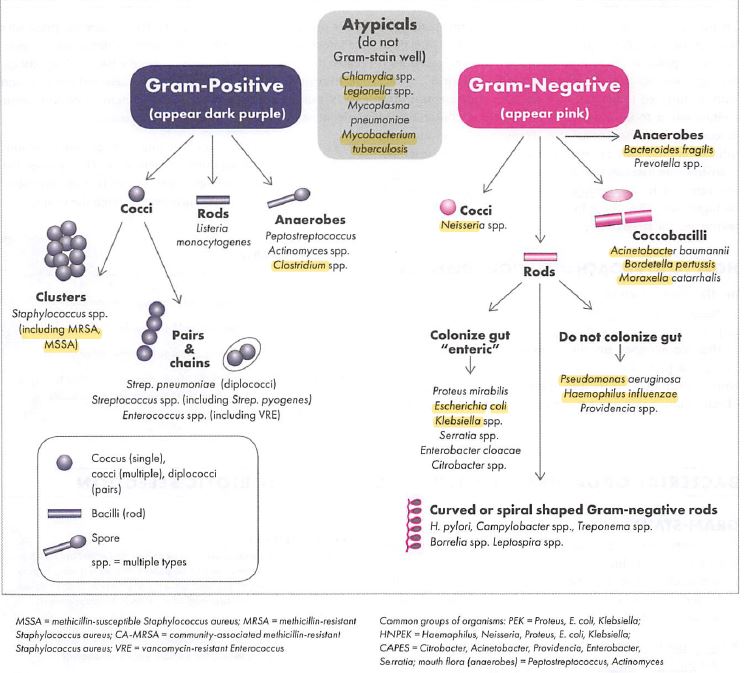
- Gram-positive: thick cell wall (peptidoglycan, in-between phosphor-bilayers), stain dark purple.
- Gram-negative: thin cell wall, stain pinkish.
- Atypical: no cell wall, does not stain well.
- Minimum inhibitor concentration (MIC): lowest drug concentration that prevents microbial growth.
- Minimum bactericidal concentration (MBC): lowest drug concentration that reduces bacterial density by 99.9%.
- Synergy: 2 or more agents produce a greater effect; useful in treating invasive infections. E.g: aminoglycoside with beta-lactams to treat gram+ infections (endocarditis), beta-lactam allows AMG to penetrate the cell wall, and reaches ribosomes.
Lab abnormality:
- The Coombs test is used to distinguish autoimmune (positive Coombs test) and nonautoimmune (negative) disorders. g: positive Coombs test meaning the patient may experience drug-related hemolysis if the patient is bleeding, and the antibiotic should be stopped. (beta-lactamase inhibitors /PCN /cephalosporins, isoniazid, rifampin, nitrofurantoin, SMX.)
- G6PD test measures the levels of glucose-6-phosphate dehydrogenase (G6PD), which helps RBCs function normally. In patients with G6PD deficiency, antibiotics have been associated with hemolytic anemia. (nitrofurantoin, dapsone, SMX)
- Drug-induced lupus: isoniazid, minocycline, terbinafine
Hydrophilic Vs. Lipophilic
Hydrophilic
- small distribution (poor tissue penetration, don’t mistake distribution as blood vessels), renal elimination (can be nephrotoxic or accumulation), low intracellular concentration (not active against atypicals), poorer bioavailability (IV: PO is NOT 1:1)
- agents: beta-lactams (outside), AMGs, glycopeptides, polymyxins (also outside), daptomycin
- Notice these hydrophilic agents typically work in the outer part of bacteria (e.g.: cell wall, membrane), atypical has no cell wall, so hydrophilic agents would not work to kill atypical.
Lipophilic
- large distribution (good tissue penetration, cell membranes are made of lipid layers, only fat-soluble drugs can cross and get in), hepatic elimination (can be hepatotoxic or drug interactions through CYP), higher intracellular concentration (active against atypical), good bioavailability (IV: PO = 1:1)
- agents: FQs, macrolides, TCNs, rifampin, linezolid, chloramphenicol, metronidazole, azoles.
- Notice these Lipophilic agents typically work in the inner part of bacteria (e.g.: target protein, DNA),
- Lipophilic is the equivalent of fat-loving (“lipo” = lipid, “philic” = affinity, towards, knowing the root words help us figure out their function!)
Antibiotic selection
- Infection characteristics: site, severity, community or hospital acquired (hospital acquired usually involve multidrug-resistant (MDR) organisms.
- Ability to penetrate: lipophilic has better tissue penetration. Hepatically cleared antibiotics may not achieve adequate concentration in the urine (won’t work for UTI).
- A broad-spectrum is used empirically to ensure coverage of likely pathogens, and then convert to the susceptible antibiotic to reduce collateral damage, when the culture and susceptibilities become available.
Common pathogens for sites of infection
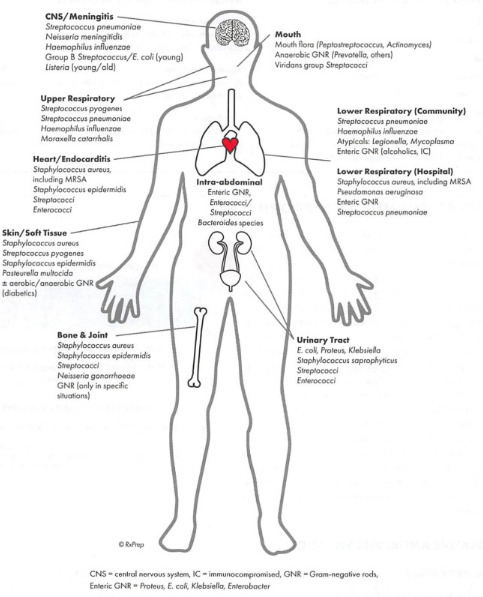
- CNS (meningitis): pneumoniae, N. meningitidis, H. influenzae, Listeria monocytogenes (in neonates, elderlies, and immunocompromised).
- Upper respiratory: pyogenes, S. pneumoniae, H. influenzae, Moraxella catarrhalis.
- Lower respiratory (community): pneumoniae, H. influenzae, atypicals.
- Lower respiratory (hospital): aureus (MRSA), Pseudomonas aeruginosa, S. pneumoniae, Enteric GNR.
- Skin/soft tissues: aureus, S. pyogenes, S. epidermidis
- Intra-abdominal: Enteric GNR, enterococci/streptococci
- Urinary tract: coli, Klebsiella, Proteus, S. saprophyticus, Streptococci, Enterococci.
- Bone and joints: aureus, S. epidermidis, Streptococci, N. gonorrhoeae.
Dose optimization
- Concentration-dependent kill (aminoglycosides): Higher doses, less frequently to maximize concentration above MIC.
- Time-dependent kill (beta-lactams): can be dosed more frequently to maximize the time above MIC. E.g: extend infusion time of beta lactams in pseudomonas reduces hospital stay.
Aminoglycosides (AMG)
- Drugs: gentamycin (Garamycin), tobramycin (Nebcin), amikacin (Amikin), streptomycin, neomycin (the only oral AMG).
- MOA: Binds to the ribosome and interferes with bacterial protein synthesis, resulting in a defective bacterial cell membrane. (Membrane is the outer part of the cell, this should help you to connect it with its property as being a hydrophilic drug, and we can speculate that it is excreted via kidney).
- Mainly against Gm- bacteria (pseudomonas), also used as synergy in Gm+ cocci (enterococcus endocarditis). Amikacin has the broadest coverage.
- Side effects: nephrotoxicity (since its hydrophilic property makes it renal elimination, accumulation can damage the kidney), ototoxicity (you’ll notice this pattern that nephrotoxicity and ototoxicity oftentimes go back-to-back, the external ear resembles the shape of the kidney. In Chinese medicine, there are many acupressure points on the ear that are beneficial for kidney health), neurotoxicity (vertigo, ataxia).
- Caution with concomitant nephrotoxic drugs: amphotericin B, cisplatin, NSAIDs, vancomycin, contrast dye, cyclosporin.
- AMGs have post-antibiotic activity: continued suppression of bacteria growth when the levels fall below the MIC. It exhibits concentration-dependent kill.
- If underweight, use actual BW, use adjusted BW if obese. (Again, try to rationalize with the lipophilic/hydrophilic property).
- Traditional Dosing: lower doses, more frequent. (Q8H for normal renal function) peak and trough level draw at the 4th
- Extended interval dosing: higher doses, less frequently. This type of dosing is less nephrotoxic and more cost-effective.
- Peak & trough levels mcg/ml
|
Gentamicin
|
5-10
|
<2
|
|
Tobramycin
|
5-10
|
<2
|
|
Amikacin
|
20 - 30
|
<5
|
Beta lactams (penicillin, cephalosporins, carbapenems)
- MOA: inhibits bacterial cell wall synthesis by binding to penicillin-binding proteins (PBP), which prevents peptidoglycan synthesis in the cell wall.
- Side effects: allergic reactions, GI (mostly diarrhea), seizure with accumulation. (Pharmacy has separate trays for PCN and sulfa drugs).
- Natural penicillin is active against gram+ bacteria, aminopenicillins have additional coverage against gram+ anaerobes, some gram-.
- DDI: Uricosuric agents (allopurinol, probenecid, cyclosporin) can increase the level of PCN by interfering with renal excretion, it is desirable sometimes if we want synergistic effects; beta-lactams can enhance effects of warfarin (inhibit vitamin K clotting factors production); May decrease the effectiveness of oral contraceptives.
Penicillin
- Mainly active against Gm+ cocci (Staph, Strep). No atypical coverage.
- Natural penicillin: Penicillin VK (Veetids)
- Aminopenicillin (extra amino group): amoxicillin (Amoxil, Moxatag), amoxicillin/clavulanic acid (Augmentin), ampicillin/sulbactam (Unasyn): combination with a beta-lactamase inhibitor provides broader spectrum, they cover Streptococci, Enterococci and Gram+ anaerobes, and some Gram- (HNPEK).
- Minimum amount of beta-lactamase inhibitor is used to ↓ diarrhea.
- Extended spectrum PCN: piperacillin/tazobactam (Zosyn), the only PCN active against Pseudomonas. It covers the same organisms as AminoPCN/beta-lactamase plus more Gram- bacteria.
- Antistaphylococcal PCN: nafcillin (a vesicant, prefer central line administration, use cold compress or hyaluronidase injections), oxacillin, and dicloxacillin, they have enhanced coverage against methicillin-susceptible Staphylococcus aureus (MSSA), and don’t need renal dose adjustment.
- Penicillin G (Bicillin L-A) is for syphilis (STD).
- Penicillin VK (Veetids): drug of choice in sickle cell disease.
Cephalosporins
- Drugs: Cephalexin (Keflex), Cefazolin (Ancef), Cefuroxime (Ceftin, Zinacef IV), Cefdinir (Omnicef), cefepime (Maxipime), Ceftaroline (Teflaro).
- 1st and 2nd generations cover gram+ cocci (Strepto, Staphyl for MSSA, therefore drug of choice for skin infection and surgical prophylaxis; some gram- coverage), 3rd, 4th, 5th generation have more gram- activity (pneumonia, meningitis, etc.).
- 3rd generation has two groups: group 1 (ceftriaxone, cefotaxime) covers more resistant staphylococci; group 2 (ceftazidime) lacks gram+ activity but covers Pseudomonas, the newer beta-lactamase inhibitor combo (ceftazidime/avibactam, ceftolozane/tazobactam) have added activity against MDR Pseudomonas and MDR gram- rods.
- 4th generation only includes cefepime: broad gram- coverage (HNPEK, CAPES and Pseudomonas).
- 5th generation only includes ceftaroline (Teflaro): similar gram- activity to ceftriaxone (3rd) but broad gram+ coverage, and is the only beta-lactam that has MRSA coverage.
- Cefotetan has a N-methylthiotetrazole (NMTT) side chain: ↑ risk of bleeding (hypoprothrombinemia, inhibits platelet aggregation) and disulfiram-like reaction with alcohol intake: cefamandole, cefmenoxime, cefmetazole, cefonicid, ceftriaxone,
cefuroxime, cefamandole, cefmetazole, cefoperazone (Cefobid), cefotetan (Cefotan), and latamoxef (moxalactam).
- Ceftriaxone: drug of choice for gonorrhea. Do not use in neonates: hyperbilirubinemia (biliary sludging).
- DI: Drugs decrease stomach acid may reduce bioavailability of some cephalosporins (Antacid, H2RA, PPI)
- No need renal dose adjustment: cefoperazone (Cefobid), ceftriaxone (Rocephine).
Carbapenems
- Drugs (IV only): ertapenem (Invanz), imipenem/cilastatin (Primaxin), meropenem (Merrem), doripenem (Doribax)
- Broad spectrum (most gram+, gram- including ESBL-producing and anaerobic coverage); Reserved for MDR gram- infections; No coverage in atypical, MRSA, VRE.
- Common use: polymicrobial infection (diabetic foot), empiric for when resistant organisms suspected, resistant Pseudomonas or Acinetobacter infection (except ertapenem not active against Pseudomonas, Enterococcus or Acinetobacter).
- Side effect: similar to other PCNs, lower seizure threshold (↓ concentration of valproic acid), caution with other drugs ↓ seizure threshold (bupropion, tramadol, quinolone, ganciclovir etc.)
- Cilastatin prevents elimination of imipenem from kidney.
Monobactam
- Drug: Azetreonam (Azactam)
- MOA: similar to beta-lactam, inhibits cell wall by binding to PBP, NO cross reactivity with beta-lactam (alternative for beta-lactam allergy)
- Covers many gram- organisms (including pseudomonas), no gram+ or anaerobe.
Fluoroquinolone (FQ)
- Agents: Ofloxacin (Floxin), norfloxacin (Noroxin), ciprofloxacin (Cipro, Proquin, Ciloxan, Cetraxal), levofloxacin (Levaquin, eye drops- Iquix/Quixin), gatifloxacin (Zymar), moxifloxacin (Avelox, Vigamox, Moxeza), gemifloxacin (Factive), norfloxacin(Noroxin), enoxacin(Penetrex).
- MOA: Inhibits DNA topoisomerase and DNA gyrase, promotes breakage of DNA. Concentration dependent kill; Active against Gm+, Gm-, some atypical.
- Side effect and warnings: tendon inflammation/rupture (risk increase with corticosteroid use, organ transplant, elderly, may cause cartilage damage in immature animals, avoid in children), peripheral neuropathy, hypo/hyperglycemia, photosensitivity, crystalluria, psychiatric disturbance, QT prolongation, seizure.
- Respiratory activity: moxi/gemi/levofloxacin (due to enhanced coverage of pneumoniae).
- Ciprofloxacin, levofloxacin: enhanced gram- coverage, and is often used in combination to treat Pseudomonas.
- Moxifloxacin is the only FQ that cannot treat UTI (does not reach adequate concentration in urine), and no need renal dose adjustment.
- Delafloxacin is a new FQ that can treat MRSA.
- Drug interactions:
- Chelation (Antacid, avoid dairy Mg, Al, Ca, iron, Zn, MVIs), didanosine, sucralfate (Al), bile acid resins.
- May ↑ levels of warfarin, sulfonylureas, QT-prolonging drugs.
- Probenecid/NSAID (renal clearance) can ↑ FQ level.
- Cipro is a potent IA2 inhibitor.
Macrolides
- Agents: Azithromycin (Zmax, ophthalmic drop: Azasite), Clarithromycin (Biaxin), Erythromycin (EES, Ery-tab), telithromycin (Ketek)
- MOA: binds 50s ribosome subunit, inhibits RNA-dependent protein synthesis; Excellent atypical coverage (Legionella, Chlamydia, Mycoplasma and Mycobacterium avium complex) and Haemophilus; drug of choice for respiratory infections (e.g: CAP) and some STD (Chlamydia, Gonorrhea)
- Side effect: GI (most with erythromycin due to ↑ gastric motility), taste perversion; Warnings: liver dysfunction, QT prolongation.
- Telithromycin SE: visual disturbance, acute hepatic failure, adjust dose in renal impairment; Blackbox warning: do not use in myasthenia gravis, cause respiratory failure; Contraindicated in history of hepatitis or jaundice from macrolides.
- Azithromycin 2g x 1 is to treat Gonorrhea (Chlamydia); Clarithromycin has a place in H. pylori treatment; Erythromycin chronic use is for gastroparesis.
- Do not refrigerate: azithromycin/clarithromycin suspension; must refrigerate: erythromycin suspension.
- Drug interaction
- Eryth/clarithromycin: major 3A4 substrates and inhibitors (contraindicated with lovastatin and simvastatin), azithromycin is a minor inhibitor.
- Caution with agents prolong QT interval (macrolides can decrease K/Mg)
Tetracycline (TCN)
- Agents: Doxycycline (Vibramycin, Oracea, Doryx, Adoxa, Periostat, 100mg q12. Oracea on empty stomach), Minocycline (Minocin, Solodyn, 50-100mg q12), Tetracycline (Sumycin, 250 - 500 mg q6)
- MOA: Inhibits bacteria protein synthesis by reversible binding to 30s ribosomal subunit.
- SE and warnings: photosensitivity, tooth discoloration (in children), GI (remain upright for 30 mins), rash, colitis, drug-induced erythematous (minocycline)
- Contraindicated in < 8 years old, pregnancy and breastfeeding (retards bone growth/skeletal development).
- Doxycycline has the broadest coverage, including respiratory (e.g: CAP), chlamydia/ gonorrhea, tick-borne/rickettsia disease, and is the drug of choice in skin infection caused by CA-MRSA, and VRE urinary tract infection.
- Minocycline is often used in skin infections like acne; Tetracycline covers many gram+, and gram- bacteria, and is used in pylori treatment.
- Drug interaction
- Antacid, Al, Ca, iron, sucralfate, bile acid resins, bismuth subsalicylate can chelate with TCN and impair its absorption (separate dose 1-2 hours before, 4 hr after)
- May enhance effects of warfarin, decrease effectiveness of oral contraceptives.
- Anticonvulsants decrease level of TCN, avoid concomitant use w/ retinoic acid.
- Tetracycline is a major 3A4 substrate.
Sulfonamides
- Drugs: sulfamethoxazole (SMX) /trimethoprim (TPM) (Bactrim, Septra) SD 400/80 or DS 800/160mg, (5:1 ratio).
- MOA: Inhibition of bacteria folic acid pathway (may need supplement with folic acid with long term use)
- Side effect: photosensitivity, ↑ K, hemolytic anemia (due to reduced folic acid, identified with a positive Coombs test), GI, Skin reactions, crystalluria (drink plenty water).
- Warning: sulfa allergy, do not use in G6PD deficiency, skin reactions (SJS).
- Common use: Gram+ (CA-MRSA skin infection), good gram- and opportunistic infection (PCP).
- UTI: BID x 3 days
- Drug interactions: Moderate inhibitor of 2C8, 2C9 (caution with warfarin).
Gram+ coverage:
- Glycopeptide (vancomycin), lipoglycopeptide (-vancin), daptomycin, Synercid
Glycopeptide
- Drugs: Vancomycin (Vancocin)
- MOA: A glycopeptide, works by inhibiting bacterial cell wall synthesis by binding to D-alanyl-D-alanine (block peptidoglycan polymerization). Exhibit time dependent kill; Only used to treat gram+ infections, most commonly MRSA.
- The oral form is ONLY used to treat C. diff (125 - 500mg QIDx10 days); The IV form is the drug of choice for MRSA. (15-20mg/kg Q8-12)
- Warnings: mostly related to infusion rates NOT blood levels, including nephrotoxicity, red man syndrome (caused by histamine release lead to maculopapular rash due to rapid infusion, this is NOT allergy, prevent by infusing slowly), hypotension (from rapid infusion).
- Adverse effects have become less and less due to the purer formulations in the market.
- Caution with concurrent nephrotoxic drugs (AMGs, amphotericin B, cisplatin, polymyxins, cyclosporine/tacrolimus, loop diuretics, NSAIDS, radio contrast dye)
- Trough level at steady state is drawn usually 30 mins before the 4th or 5th dose), higher concentration is required for severe infections (such as bacteremia, pneumonia, meningitis, osteomyelitis, 10-20 mcg/ml), otherwise, >10mcg/ml in most patients.
Lipoglycopeptides
- Drugs: Telavancin (Vibative), Dalbavancin (Dalvance), Oritavancin (Orbactiv)
- MOA: inhibits cell wall synthesis by binding to D-alanyl-D-alanine, concentration-dependent kill.
- Warnings: nephrotoxicity, red man syndrome with rapid IV, falsely elevate coagulation tests (heparin is not a contraindication).
- Oritavancin and dalbavancin: One time only dose due to a long half-life.
- DI: avoid drugs with QT prolongation.
Daptomycin (Cubicin)
- MOA: a cyclic lipopeptide binds cell membrane causing rapid depolarization and inhibits intracellular activities.
- Most gram+ coverage including MRSA and Enterococci (VRE, both faecium and E. faecalis) concentration-dependent kill.
- Warnings: rhabdomyolysis and myopathy, falsely ↑ INR/PT.
- SE: ↑ CPK (requires frequent monitoring).
- Injection only.
Oxazolidinones
- Drugs: linezolid (Zyvox), tedizolid
- MOA: binds 50S subunit of ribosome, inhibits bacteria translation and protein synthesis. Similar coverage to vancomycin, plus VRE ( faecium, E. faecalis).
- SE: ↓ platelets Hgb/WBC.
- Warnings: myelosuppression (anemia, leukopenia, pancytopenia, and thrombocytopenia, duration related), serotonin syndrome (they are reversible monoamine oxidase inhibitors, avoid tyramine foods, do not use within 2 weeks of MAOI), optic neuropathy, hypoglycemia, ↑ BP (avoid adrenergic drugs for hypertensive effect).
- Uncomplicated skin infections are treated with PO or SUSP. Complicated are treated with IV Q12 hours.
- No dose adjustment required for renal impairment. IV:PO = 1:1.
- Tedizolid: a relatively new agent in this drug class; May have less SE compared to linezolid including less myelosuppression (hence CBC monitoring not required), and slightly better coverage to gram+.
Quinupristin/dalfopristin (Synercid)
- MOA: A streptogramin binds 50s ribosome subunit, inhibits protein synthesis. Covers most gram+ (MRSA, enterococcus faecium VRE, but not E. faecalis).
- Not well tolerated, limited to vancomycin-resistant E. faecium.
- SE: arthralgia/myalgia, hyperbilirubinemia.
Broad spectrum antibiotics
Tigecycline (Tygacil)
- MOA: a glycycycline, binds 30s ribosome subunit, inhibits protein synthesis. Related to tetracyclines (a derivative of minocycline). Broad spectrum coverage of gram+, including MRSA, and enterococci (VRE), gram-, anaerobes, atypical. No activity against pseudomonas.
- Do not use in blood infection (lipophilic, do not achieve enough concentration in blood)
- DI: ↑ INR in patients taking warfarin.
Polymyxin
- Consists of two drugs (colistin, polymyxin B)
- Covers gram- bacteria (Pseudomonas), due to toxicity, generally reserved for MDR gram- pathogens.
- Warning: nephrotoxicity, neurotoxicity.
- DI: use with other nephrotoxic drugs can increase nephrotoxicity.
Chloramphenicol
- MOA: binds 50s ribosome subunit, inhibits protein synthesis.
- rarely used due to boxed warning: fatal blood dyscrasias (aplastic anemia, thrombocytopenia).
- Cause myelosuppression, gray syndrome.
Miscellaneous
Clindamycin (Cleocin)
- MOA: a lincosamide binds 50s ribosome subunit, inhibits protein synthesis. Activity against aerobic and anaerobic gram+. (no coverage against gram-).
- SE: N/V/D, colitis.
- Treating community MRSA orally.
- Pregnancy B, no need renal dose adjustment.
- Topical brand names: Evoclin, Clindagel. Vaginal names: Clindesse, Cleocin.
Metronidazole (Flagyl, Metrogel), Tinidazole (Tindamax)
- MOA: Cause loss of DNA structure, inhibits protein synthesis.
- Activity against anaerobes and protozoal. Drug of choice for bacterial vaginosis, trichomoniasis, intra-abdominal infections.
- Warning: CNS effects (seizure, peripheral neuropathy)
- SE: GI, metallic taste, furry tongue, glossitis, discolor urine (reddish brown).
- Pregnancy category B (but CI in 1st trimester)
- Lipophilic drug, IV:PO = 1:1, no need renal dose adjustment.
- Disulfiram reaction (abdominal cramping, N/V/HA, flushing) with alcohol intake, no EtOH during and 3 days after last dose).
- Can ↑INR in patients taking warfarin.
Rifaximin (Xifaxan)
- Inhibits RNA synthesis, structurally related to rifampin.
- Covers Coli, treats Traveler's diarrhea (200mg TID x 3 days) and irritable bowel syndrome with diarrhea (550mg TID x 14 days)
Mupirocin (Bactroban)
- A nasal ointment used to eliminate MRSA colonization of nares.
Urinary agents
Nitrofurantoin (Macrobid BID, Macrodantin QID)
- Bacterial cell wall synthesis inhibitor, for uncomplicated UTI.
- Contraindicated in renal impairment (CrCl<60 ml/min) and pregnancy (at term)
- Warning: hemolytic anemia (caution in a positive Coombs test & G6PD deficiency), peripheral neuropathy and pulmonary toxicity in long term use.
- SE: brown urine discoloration, GI upset (take with food).
Pregnancy:
- Anatomical changes increase the risk that bacteria in the urine can progress to more severe infections, it is vital to treat UTI in pregnancy even if asymptomatic
- Avoid: quinolones (cartilage toxicity), TCN (teratogenic).
- By trimester: Bactrim (avoid 1st trimester: neural tube defects, 3rd trimester: high bilirubin); Macrobid (avoid 1st trimester: heart defects, cleft lips), feel comfortable if you see an Rx prescribed during pregnancy, but avoid during last month: hemolytic anemia in newborn.
- beta lactam: generally safe. (e.g: amoxicillin, cephalosporins).
- fosfomycin (Monurol): just one 3g dose, can be used in any trimester, however expensive.
Community acquired MRSA (CA-MRSA)
- SMX/TMP, doxycycline/minocycline, clindamycin, Linezolid
MRSA
- Ceftaroline, vancomycin (and other -vancins), daptomycin, tigecycline, quin/dalf, Linezolid
Pseudomonas Aeruginosa
- Aminoglycosides, piperacin/tozabactam, carbapenems (NO ertapenem), cefepime/ceftazidime, combo cepholosporin (with beta-lactamase), cipro/levofloxacin, Aztreonam, polymyxin. (NO macrolide!)
VRE Faecium
- Penicillin G/Ampicillin, Linezolid, Daptomycin, tigecycline, Quin/dalf
VRE Faecalis
- Penicillin G/Ampicillin, Linezolid, Daptomycin, tigecycline
Acinetobacter
- Carbapenems (NO ertapenem)
Perioperative
- Primary organisms on the surface of skin: Streptococci and Staphylococci, 1st generation cephalosporin (cefazolin IV) is common used as prophylactic antibiotic.
- Dental prophylaxis: amoxicillin PO 2g before procedure (or IV ampicillin, cefazolin); Alternatives for PCN allergy: clindamycin or azithro/clarithromycin.
Skin and soft tissues
- Superficial infections (mild): impetigo, furuncles (boil), and carbuncles (a group of furuncles). Treatment include warm wet compress to remove dried crusts, topical antibiotic (mupirocin), or PO cephalexin for numerous lesions (to cover MSSA); if non-responsive, change to CA-MRSA coverage: SMX/TMP, doxycycline.
- Non-purulent infections (moderate): subcutaneous tissues (cellulitis). Treatment: Oral antibiotics that covers MSSA (cephalexin, clindamycin).
- Purulent infections (severe): abscesses; Use antibiotics with CA-MRSA coverage (SMX/TMP, doxycycline); for severe purulent, use antibiotics with MRSA coverage (vancomycin and the -vancins, daptomycin, linezolid, ceftaroline); for deadly necrotizing fasciitis, use vancomycin + beta-lactam (Zosyn, or imipenem/cilastatin or meropenem)
Meningitis
- Classic presentation: severe headache, stiff neck (nuchal rigidity), and altered mental status.
- Mostly caused by virus but can be caused by these 3 most common bacteria: pneumoniae, N. meningitidis, H. influenzae.
Upper respiratory
- Acute otitis media is the most common form.
- Observation for 48-72 hours for non-severe (< 102.2 o)
- 1st line: high dose amoxicillin 80 – 90 mg/kg/day in 2 divided doses, or Augmentin 90mg/kg/day in 2 divided doses. The least amount of clavulanate is used to prevent diarrhea (Augmentin ES 600 has a lower ratio of clavulanate)
- If PCN allergy, use a cephalosporin.
- Prevention: pneumococcal conjugate vaccine (PCV13, Prevnar 13) for 2 months of age and up, and annual influenza for age >= 6 months.
Lower respiratory
Acute bronchitis
- Mostly caused by respiratory viruses: RSV, adenovirus, rhinovirus, coronavirus, influenza virus. In more severe cases (purulent sputum), can be caused by bacteria.
- Mild to moderate: azithromycin, clarithromycin or SMX/TMP
- Severe: Augmentin is preferred.
Pneumonia
Community acquired pneumonia (CAP)
- Common pathogens: pneumoniae, M. pneumoniae, H. influenzae.
- No recent antibiotic use (past 3 months): 1. macrolide (azi/clari/erythromycin), or 2. doxycycline
- Recent antibiotic use (risk of drug-resistency): 1. (macrolide or doxycycline) + beta-lactam or 2. Respiratory FQ (moxi/gemi/levo)
- Inpatient CAP: monotherapy is not recommended for patients who are more ill, same regimen as above.
- If patient has risk for Pseudomonas, the regimen should cover Pseudomonas and S. pneumoniae. (Zosyn, cefepime, meropenem, or levofloxacin)
Hospital acquired
- Pathogens in hospital acquired pneumonia (HAP) and ventilator-associated pneumonia (VAP): P. aeruginosa, Acinetobacter, gram- rods (Enterobacter, E. coli, Klebsiella); if MDR, add MRSA coverage (vancomycin, linezolid)
Tuberculosis (TB)
- Caused by mycobacterium tuberculosis. (An aerobic, non-spore forming bacillus).
- Highly contagious, diagnosed by tuberculin skin test PPD (raised bump 48-72 hrs after injection); false positive occurs in those who received BCG vaccine. Active TB must be isolated in single rooms.
- Latent TB: INH 300mg QD x 9 months, or rifampin x 4 months (rifampin + pyrazinamide no longer recommended due to liver damage).
- Active TB: intensive phase: 4 drugs (RIPE) x 2 months; continuation phase: 2 drugs (INH, rifampin) x 4 months.
- Direct observed therapy (DOT) is dosed 2 - 3 times per weekly instead of daily, to increase adherence.
- Drugs: RIPE, all ↑LFT and may cause liver damage.
- Rifampin: on empty stomach; orange/red discoloration of bodily secretion; a potent inducer (can be replaced by rifabutin for less Dis).
- Isoniazid (INH): on empty stomach; may cause neurotoxicity (increase intake of V-B6, folic acid, niacin, Mg), lupus (DILE), hemolytic anemia (risk is detected by positive Coombs test).
- Pyrazinamide: ↑ uric acid levels.
- Ethambutol: vision damage (optic neuritis), confusion/hallucinations.
- Vb-6 (pyridoxine): reduce risk of neuropathy
- Streptomycin: Blackbox warning: neuro/nephrotoxicity/ototoxicity (IV), respiratory paralysis; increase nephrotoxicity with nephrotoxic agents.
Endocarditis
- Infection of the inner tissue of the heart, especially the valves, patients with prosthetic heart values, prolonged IV access are at highest risk. The condition can be fatal if not treated.
- Echocardiogram is used to visualize the vegetation, and blood culture is to confirm infection.
- 3 most common pathogens: Staphylococci, Streptococci, and Enterococci.
- Empiric treatment: vancomycin and ceftriaxone x 4-6 weeks, gentamicin is used for synergy for more resistant organisms.
Intra-abdominal
- Likely pathogens: Streptococci, enteric Gr- organisms (PEK)
- Drug of choice: ceftriaxone 5-7 days.
C. diff
- All antibiotics overuse carries risk of C.diff, some has higher risk such as clindamycin.
- first-line: metronidazole or vancomycin PO.
- Vancomycin oral solution (Firvanq): QID X 10 days. If recurrence, can use an extended taper vancomycin therapy as oppose to abrupt stop.
- Fidaxomicin (Dificid): inhibits DNA polymerase, for severe strains or patients who fail oral vancomycin, very expensive
- Fecal transplant for patients has 3 or more C. diff episodes, failed antibiotic treatment, to restore healthy GI flora.
- To prevent C.diff: limiting antibiotics, stopping unnecessary PPIs, handwashing with soap and water. How about probiotics? They may help, so don’t discourage the use if patients are willing to try.
Traveler’s diarrhea
- Often caused by contaminated food or water, mostly are bacterial cause.
- Common bacterias: coli, C. jejuni, Shigella, Salmonella spp.
- Common viruses: rotavirus, Protozoa, Giardia, Entamoeba histolytica, etc.
- Azithromycin is the preferred treatment if dysentery is present (bloody diarrhea), alternatives are quinolones or rifaximin.
UTI
- Can include lower part of urinary tract: bladder (cystitis) and urethra, or upper urinary tract: kidney (pyelonephritis).
- Occur more common in females due to shorter route from urethra to bladder. Can be classified as uncomplicated (non-pregnant, no comorbidities) or complicated (male, pregnant woman, urologic abnormalities, or indwelling catheter).
- Uncomplicated: nitrofurantoin BID x 5 days (or SMX/TMP DS BID x 3 days, or Fosfomycin x 1 dose); alternatives: cipro/levofloxacin or beta-lactam (Augmentin, cephalosporin)
- Quinolones are used for more upper stream like pyelonephritis as verse to cystitis; Note moxifloxacin does NOT reach high urine concentration and is not effective as an urinary agent.
- Complicated: similar treatment to pyelonephritis, use carbapenem if ESBL producing bacteria.
- Dysuria (pain and burning with urination): use a urinary analgesic phenazopyridine (Pyridium RX, Azo OTC), which can cause red-orange discoloration of bodily fluids.
Bacteriuria in pregnancy
- Pregnant women must be treated even if no symptoms, otherwise the infection can progress to pyelonephritis, premature birth or neonatal meningitis.
- Preferred agent is beta-lactam (Augmentin, or cephalosporin), alternatives are nitrofurantoin and SMX/TMP for PCN allergy, but avoid in 1st trimester
STD
- Syphilis: Penicillin G (Bicillin L-A) IM x 1; alternative for PCN allergy: doxycycline.
- Gonorrhea: ceftriaxone IM x 1 + azithromycin (or doxycycline); do not use monotherapy which can lead to resistance; azithromycin part treats chlamydia as it often go together with gonorrhea.
- Chlamydia: azithromycin 1 gram PO x 1 (or doxycycline).
- Bacterial vaginosis: metronidazole PO or PV
- Trichomoniasis: metronidazole PO
Rickettsial diseases
- Bacterial infection spread by ticks, fleas and lice.
- Common agent: doxycycline
Fungal infections
- Fungus: yeast (Candida species: albican is the most common and susceptible), mold (Aspergillosis, Zygomycetes), dimorphic fungi (exist as mold at lower temp and as yeast at higher temp).
Azoles
- Drugs: Fluconazole (Diflucan), Ketoconazole (Nizoral, Extina, Xolegel, Kuric), Itraconazole (Sporanox), Voriconazole (Vfend), Posaconazole(Noxafil).
- MOAs: decreases ergosterol synthesis and inhibit cell membrane formation.
- SE: ↑ LFT, QT prolongation; BBW: CV events such as CHF (Itraconazole).
- Capsule form has low bioavailability and must be taken with food, requires acidic gastric environment; oral solution is more bioavailable.
- Strong 3A4 inhibitors, lots of drug interactions.
- Voriconazole: on empty stomach; SE: visual changes, CNS toxicity. Notable for drug interactions. Drug of choice for Aspergillus.
- Itraconazole: contraindicated in HF.
- All except fluconazole requires renal dose adjustment.
- Itra/ketoconazole: pH-dependent absorption, most effective in acidic environment.
Echinocandins
- Drugs: Capsofungin (Cancidas), Micafungin (Mycamine), Anidulafungin (Eraxis).
- MOA: inhibit synthesis of beta 1,3-D-glucan, major component of fungal cell wall. Treat most Candida and
- SE: ↑ LFT
- Injection only, once daily, no need renal dose adjustment.
Amphotericin B (Ambisome, Abelcet)
- Broad spectrum; covers yeasts, molds and dimorphic fungi. Can treat serious fungal infection such as:
- Many toxicities, including nephrotoxic.
- Injection only; lipid formulation reduce infusion reactions and nephrotoxicity.
Other antifungal
- Griseofulvin: Less effective than systemic agents (azoles or terbinafine), and requires prolonged use; SE: ↑ LFT, photosensitivity; Take with a fatty meal to increase absorption.
- Terbinafine (Lamisil): hepatotoxicity.
- Clotrimazole (Mycelex): ↑ LFT.
- Nystatin: commonly treats oral thrush, minimal GI absorption, formulations are mostly topical.
Viral infection
Treatment by 2 ways: either directly inhibit viruses, or augment/modify host immune response (immunomodulators)
Influenza
- Neuraminidase inhibitors (oseltamivir, zanamivir) inhibit an enzyme to prevent release of viral particles.
- Warnings: neuropsychiatric events (Tamiflu), bronchospasm (zanamivir -Relenza Diskhaler)
- Most effective to start within 48 hours of illness.
Herpes simplex virus (HSV)
- HSV-1 (oral): Denavir cream (pencyclovir), acyclovir (Zovirax cream), OTC Abreva(docosanol) for cold sore.
- HSV-2 (genital): Acyclovir (Zovirax, frequent dosing), valacyclovir (Valtrex, prodrug of acyclovir), famcyclovir (Famvir, prodrug of penciclovir)
- Varicella-zoster virus (VZV): chicken pox or shingle.
Cytomegalovirus (CMV)
- Occurs in immunocompromised (HIV, transplants)
- Treatment: ganciclovir, valganciclovir (class side effects: myelosuppression)
- Foscarnet and cidofovir reserved for recurrent CMV.
Opportunistic infection
- Immunocompromised patients (HIV CD4 count < 200, transplants, chemotherapy, prolonged high dose steroids, asplenia) are at high risk.
- A variety of pathogens include bacteria, fungi, viruses, and protozoa.
- CD4 count < 200 cells/mm3: at higher risk of developing Pneumocystis jiroveci (previously carinii) pneumonia (PCP).
- <100 cells/mm3: at risk for Toxoplasma gondii (causative agent of toxoplasmosis).
- < 50 cells/mm3: at higher risk for Mycobacterium avium complex (MAC) and cytomegalovirus disease (CMV):
- Candidiasis: fluconazole, itraconazole.
- PCP: SMX/TMP.
- MAC: azithromycin + ethambutol
- CMV: 1st line is valganciclovir (Valcyte), ganciclovir; Foscarnet and cidofovir reserved for recurrent CMV.
- Toxoplasmosis: pyrimethamine + leucovorin + sulfadiazine (leucovorin is the rescue agent to reduce myelosuppression associated with pyrimethamine).
Avoid alcohol
- Most medications should avoid concomitant alcohol use, however more so with the following list.
- Disulfiram(Antabuse): acts as an enzyme inhibitor (acetaldehyde dehydrogenase), preventing the metabolism of acetaldehyde into acetic acid, and is used in the treatment of alcoholism.
- A disulfiram-like drug causes hypersensitivityto alcohol (N/V, flushing, dizziness, throbbing headache, chest and abdominal discomfort, and general hangover-like symptoms). Effects are caused by accumulation of acetaldehyde: a toxic metabolite of alcohol.
- Many disulfiram-like drugs are antibiotics:
- Cephalosporins: cefamandole, cefmenoxime, cefmetazole, cefonicid, cefoperazone, cefotetan, ceftriaxone, cefuroxime, and latamoxef (moxalactam).
- Metronidazole, sulfonamides, sulfonylurea
- Oral corticosteroid, NSAIDs
- Phenytoin
Photosensitivity
- sulfonamides, fluoroquinolones, and tetracyclines
NO need renal dose adjustments
- Most antibiotics require renal dose adjustment.
- Formula: Cockcroft gault: CrCl = [ (140 - age) x kg ] / (72 x SCr) (x 0.85 if female)
- Anti-staphylococcal penicillin (e.g: Oxacillin, nafcillin)
- Ceftriaxone/cefoperazone from cephalosporins
- Clindamycin
- Doxycycline from TCN
- Macrolides (azithromycin, erythromycin only)
- Metronidazole, tinidazole
- Moxifloxacin from quinolones
- Linezolid
Diluent compatibility
- D5W only: Quin/dalf, SMX/TMP, amphotericin B
- NS only: ampicillin, ampicillin/sulbactam, ertapenem (notice they are all beta lactams)
Quiz
- The final dosage form of which of the following drugs could not be an elixir? (Select ALL that apply)
- Cefobid
- Moxalactam
- Flagyl
- cefoperazone
- Amoxicillin
- A pharmacist receives a new prescription for Augmentin 500 mg. The prescription reads 1 tab po bid x 10 days. A technician in the pharmacy fills and processes the prescription using 250 mg of Augmentin instead, since the pharmacy is out of stock of 500 mg Augmentin tablets. The pharmacist who is doing the final check of the prescription should:
- Fill the prescription as it is.
- Call the physician and get approval regarding this switch.
- Not fill the prescription.
- Fill the prescription but counsel and inform the patient about this switch.
Which of the following medications should NOT be given to a 1-year-old patient?- Amoxicillin
- Cephalexin
- Clindamycin
- Azithromycin
- Tetracycline
- Which of the following medications would be appropriate to treat Pseudomonas aeruginosa?
- Oxacillin
- Cefepime
- Ceftriaxone
- Clarithromycin
- Clindamycin
- A patient admitted to the hospital is diagnosed with aspergillosis. Which of the following antimicrobial agents would be MOST appropriate to initiate in this patient?
- Tigecycline
- Caspofungin
- Chloramphenicol
- Nystatin
- A patient taking which of the following antimicrobial agents should be counseled to avoid prolonged sun exposure because of the risk of photosensitivity? (Select ALL that apply.)
- Bactrim
- Erythromycin
- Clindamycin
- Gemifloxacin
- Minocycline
- Which of the following drugs used in the treatment of tuberculosis can cause orange-red discoloration of a patient’ s urine?
- Isoniazid
- Ethambutol
- Pyrazinamide
- Rifampin
- Streptomycin
- A woman diagnosed with a sexually transmitted disease picks up her antibiotic prescription at her local pharmacy. The pharmacist counsels her that she should not drink alcoholic beverages while taking this medication because it may lead to an unpleasant reaction. Which of the following antibiotics has MOST likely been prescribed for this patient?
- Z-pak
- Cefixime
- Doxycycline
- Flagyl
- Penicillin VK
- An 85-year-old female patient has been hospitalized with an infection. She has a creatinine clearance of 25 mL/min. Which of the following antibiotics does NOT need to be dose-adjusted in this patient?
- Ceftriaxone
- Amikacin
- Meropenem
- Zosyn
- Vancomycin
- Which of the following antibiotics is the first-line therapy for Pneumocystis jirovecipneumonia?
- Chloramphenicol
- Azithromycin
- Ciprofloxacin
- Voriconazole
- Bactrim
- Acyclovir is available in which of the following formulations? (Select ALL that apply.)
- Tablet
- IV Injection
- Oral suspension
- Topical ointment
- Transdermal patch
Answers
- Elixir contains a small % of alcohol. ABCD have been found to interact with alcohol and may produce disulfiram-like reactions. Ethanol is converted to acetaldehyde by an enzyme (alcohol dehydrogenase), which is subsequently converted to acetic acid by aldehyde dehydrogenase enzyme. Accumulation of acetaldehyde is responsible for producing hot flashing, throbbing headaches and disulfiram-like reactions.
- Since both the 250 mg and 500 mg tablets of amoxicillin/clavulanate potassium contain the same amount of clavulanic acid (125 mg, as the potassium salt), two amoxicillin/clavulanate potassium 250 mg tablets are not equivalent to one 500 mg amoxicillin/clavulanate potassium tablet.
- Tetracycline should not be given to children, as it can cause enamel hypoplasia or permanent tooth discoloration.
- Cefepime, a 4th-generation cephalosporin, is the only antibiotic listed that would treat an infection caused by Pseudomonas.
- Aspergillosis is a serious fungal infection. Nystatin is used topically for local infections caused by Candida or as an oral suspension for thrush. Caspofungin is administered IV and can be used for the treatment of aspergillosis.
- ADE. Sulfonamides, fluoroquinolones, and tetracyclines are associated with an increased risk of photosensitivity.
- Rifampin can cause an orange-red discoloration of all bodily fluids.
- Metronidazole (Flagyl) should not be taken with alcohol as this may lead to a disulfiram-like reaction, which manifests as flushing, headache, N/V, or chest/abdominal pain. Although patients generally should avoid taking medications with alcohol, the concomitant use with metronidazole specifically cause an unpleasant reaction.
- Ceftriaxone is eliminated via biliary and renal excretion. Therefore, the dose not need to be adjusted in patients with renal impairment. Amikacin and vancomycin are nephrotoxic antibiotics.
- Pneumocystis jirovecipneumonia is an opportunistic infection. Trimethoprim/sulfamethoxazole (Bactrim) is the drug of choice if the patient does not have a sulfa allergy. Other alternatives in treating opportunistic infections are: dapsone, pentamidine, or atovaquone.
- Acyclovir is available as a capsule, injection, suspension and a topical ointment. Acyclovir is not available as a transdermal patch.
Was this page helpful?
Back to top »