Updates: Feb 24th, 2021
Dec 12th, 2019
Background
- Seizure (SZ) occurs when excitatory (activating) neurons produce a surge of electric activity in the brain. The surge can be an imbalance in neurotransmitters (inhibitory NT GABA, excitatory NT glutamate). SZ can destroy neurons and causes brain damage.
- Correcting temporary condition (high fever (common in children), electrolyte abnormality, infection, hypoglycemia, head injury etc.) can treat seizure.
- Epilepsy is a chronic seizure disorder, varies from jerking movements (tonic-clonic seizure) to memory loss of awareness (absence seizure).
- EEG is the most common diagnostic tool for epilepsy, that can show abnormal electric activity while the patient is not having a seizure.
- 3 main types: focal, generalized, and unknown onset seizures. Focal starts on one side and can spread (depending on loss of awareness, can be further classified as focal awareness SZ or focal SZ with impaired awareness); generalized starts on both sides, unknown onset is the location of the beginning of SZ is not known.
- Types based on symptoms: motor symptoms include sustained jerking movements (clonic), limp/weak muscle (atonic), and rigid tense muscle twitching (tonic). Non motor symptoms include change in sensation emotion, or cognition. Absence SZ (starring spells) is generalized SZ without motor symptoms.
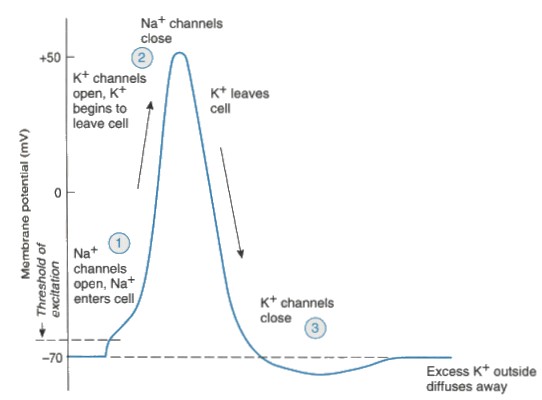
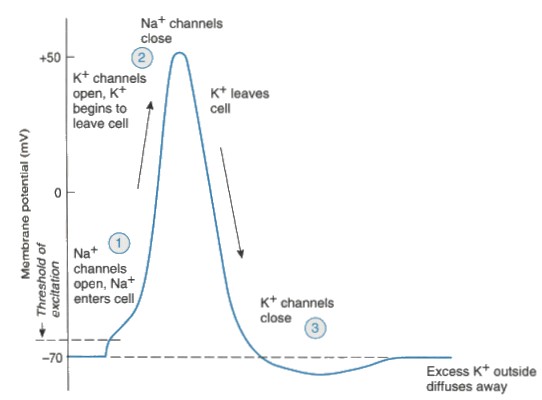
- Most of antiepileptic drugs (AED) target ion channels (Na, Ca are involved in the generation of action potential) or neurotransmitters (either ↓ excitatory NT, or ↑ inhibitory NT).
Drugs lower seizure threshold
- High dose and risk ↑ with poor renal function: antibiotics (carbapenems, quinolones), Li, meperidine, theophylline, bupropion, tramadol, clozapine, varenicline.
Acute SZ management
- Most SZs last <2 mins and do not require medical intervention. However, status epilepticus (SE) lasts > 5mins, and is an emergency. Initial treatment includes an IV benzo-diazepam (BZDs, e.g: diazepam, lorazepam), or midazolam IM if unable to get IV access.
- If unable to receive an injection, use diazepam rectal gel (Diastat, Acudial or buccal form for quick onsets). Dial and lock the prescribed dose before dispensing!
- If SZ continues after BZD, administer IV AED (fosphenytoin, valproic acid, levetiracetam).
- First aid measures: turn the person on one side this helps the airway stay open, dial 911 and time the seizure with a watch, do not hold the person down to try to stop their movements.
AEDs for chronic SZ management
- Drugs: benzodiazepam, valproic acid/divalproex (Depakote, Depakene), phenobarbital (Luminal), levetiracetam (Keppra), oxcarbazepam (Trileptal), carbamazepine AKA CBZ (Tegretol, Carbatrol), lamotrigine (Lamictal), phenytoin (Dilantin) /fospheytoin (Cerebyx), topiramate (Topamax), pregabalin (Lyrica) /gabapentin (Neurontin, Horizant ER), ethosuximide
- MOA: either ↑ GABA (inhibitory action inhibits neuron firing), or block Na channels (reduce depolarization making firing less likely, sometimes block Ca channels).
- SEs and reasoning: bone loss and ↑fracture risk (if the drug blocks Ca channels, that may leads to lower [Ca], supplement with Ca+V-d), many causes serious skin reaction (SJS, and TEN), boxed warning of suicide risk (AEDs work in the brain, so monitor mood), older AEDs have teratogenic risk (drugs that can cross placenta are highly lipophilic, valproic acid has the highest risk, phenobarb, phenytoin, CBZ, and clonazepam); Unique SEs: topiramate and zonisamide can cause reduced sweat (hypohidrosis) in young children, lamotrigine induces rash can be more common among kids. Here both the risks are higher in children, they have smaller body weight and fast blood circulation, meaning drugs can be distributed more quickly, any SEs would be more apparent compared to adults.
- DIs: Most are enzyme inducers and can reduce efficacy of oral contraceptives (use non-hormonal options), EXCEPT valproic acid, which is an inhibitor (can raise level of lamotrigine, ↑ risk of severe rash).
- AEDs are first line. AEDs must cross the blood brain barrier and depress electric activity in the brain. All AEDs are CNS depressant: dizziness, confusion, sedation, unable to coordinate movements.
- Avoid meds that can lower SZ threshold, stopping AED abruptly can lead to seizure.
- ODT, chewable, and solution make it easier for patients with difficulty swallowing.
- Broad spectrum AEDs cover various SZ types (generalized and focal SZ), narrow spectrums are used for isolated specific conditions (e.g: ethosuximide is used for absence SZ), pregabalin/gabapentin are not usually used for SZ and are commonly used for neuropathic pain.
- Family members of AEDs share similar SE:
|
Drugs
|
Adverse effect
|
|
CBZ/oxcarbazepine/eslicarbazepine
|
hyponatremia, rash, enzyme inducers
|
|
Phenobarb, primidone
|
sedation, inducer, risk of dependence/overdose
|
|
Topiramate, zonisamide
|
weight loss, metabolic acidosis, nephrolithiasis/oligohidrosis
|
Non-drug treatment
- Keto diet: high fat, low carb, normal protein diet, body breaks down fatty acid into ketone, which replaces glucose in the brain, reduce SZ frequency.
- Vagal nerve stimulation, surgical removal.
- Medical cannabis: be aware of CNS side effects of the THC component: somnolence, euphoria, etc., and CYP 1A2 induction.
Board spectrum AEDs
- Lamotrigine: BBW: serious skin reaction (slow titration), level increased level by valproic acid (which is a CYP inhibitor), the level decreased by inducer (CBZ, phenobarb/primidone, phenytoin, lopinavir/ritonavir, rifampin), estrogen-containing contraceptives.
- Levetiracetam: warnings (psychiatric symptoms) and IV:PO = 1:1 suggest its lipophilicity.
- Topiramate: also used for weight loss (Qsymia=topiramate/phentermine) and migraine prophylaxis, warnings on metabolic acidosis (bicarb imbalance), hyperthermia/oligohidrosis (reduced perspiration, avoid sun and hydrate), nephrolithiasis (kidney stone), hyperammonemia, angle closed glaucoma; ↓effectiveness of oral contraceptives.
- Valproic acid: also used for bipolar and migraine prevention. Therapeutic range: 50-100 mcg/ml, BBW: hepatic failure, teratogenicity. SE: weight gain, alopecia, thrombocytopenia, hyperammonemia (treat with carnitine), ↑LFT; weak inhibitor of 2C19, avoid using with lamotrigine (serious rash), salicylates may displace valproic acid from protein binding site.
Narrow spectrum AEDs
- Carbamazepine: also used neuralgia, bipolar disorder (Equetro); wacky SE: hyponatremia (SIADH), fetal harm, myelosuppression (agranulocytosis, aplastic anemia), teratogenic; BBW: serious skin reactions (if test positive HLA -A*3101 and HLA-B* 1502, cannot use); A potent inducer and autoinducer (induce its own metabolism); Range: 4-12 mcg/ml.
- oxcarbazepine: serious skin reactions (screen Asian descent for HLA-B*1502), hyponatremia.
- Phenobarb (C-IV), strong inducer, SE similar to alcohol (somnolence, respiratory depression), fetal harm; Range: 20-40 mcg/ml, prodrug is primidone (Mysoline).
- lacosamide (Vimpat, C-V): warning prolongs PR, ↑ risk of arrythmia.
- Phenytoin/fosphenytoin: please see the section below for more details.
Phenytoin
- warnings: extravasation (purple glove syndrome,) V-D/Ca deficiency (osteoporosis, supplement with folic acid, Ca+V-D), hepatotoxicity, lupus like syndrome, serious skin reactions (SJS, TEN, avoid in positive HLA-B*1502 genetic testing), fetal harm , gingival hyperplasia (also a side effect of verapamil).
- Toxicity similar to alcohol toxicity (CNS changes): ataxia/slurred speech/confusion, additionally a unique side effect is nystagmus (wobbly eye ball movements), diplopia.
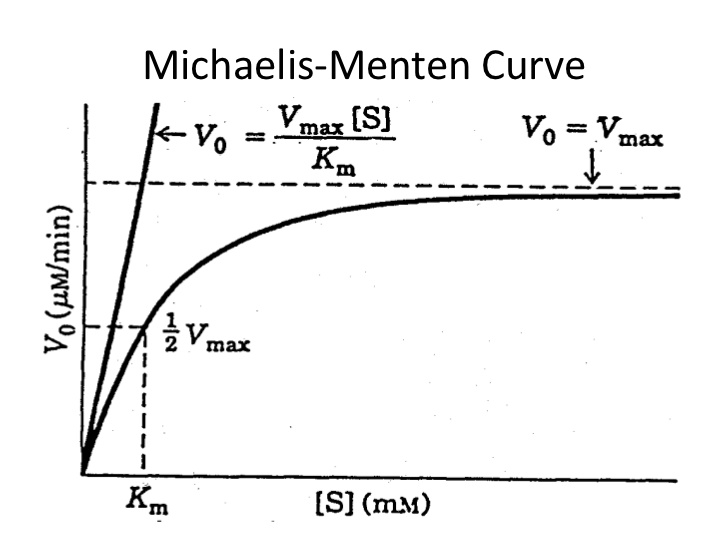
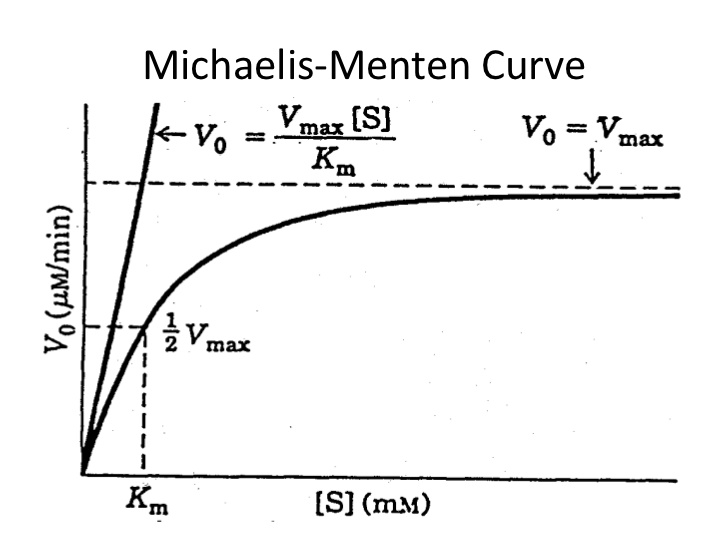
- Dosing: 100mg TID, metabolism can be saturated, a small increase in dose can cause a big increase in serum level when the enzyme have become saturated, it follows saturable Michaels-Menten kinetics (also known as zero-order kinetics:), narrow therapeutic dosing window: 10-20 mcg/mL.
- Max infusion rate 50 mg/min, mix injection in NS only and requires a filter; fosphenytoin is a pro-drug of phenytoin, can be infused faster, can mix in either NS or D5W.
- High protein-binding, it can displace other protein bound drugs. IV:PO = 1:1 (suggest lipophilic), do not give via feeding tube due to protein binding property, hold feeds 2 hr before and after.
- patients with low albumin level (< 3.5) would need dose adjustment (phenytoin level would appear artificially low). Phenytoin corrected = phenytoin measured / [(0.2 x albumin) + 0.1].
- DI: A strong inducer of several CYP enzymes.
Other AEDs
- Zonisamide (Zonegran), used for absence SZ, avoid in sulfonamide allergy, warnings: oligohidrosis/hyperthermia, nephrolithiasis;
- Vigabatrin (Sabril): Only available through REMS program (BBW: permanent vision loss).
- Pregabalin C-V / Gabapentin: SE: somnolence, peripheral edema/weight gain, mild euphoria, commonly used for neuropathic pain. Titrate dose slowly (dose-related kinetics).
- Felbamate (Felbatol): hepatic failure, aplastic anemia.
- Eslicarbazepam: acive metabolite of CBZ, ↓Na.
- clobazam ( Onfi): one of BZDs, C-IV.
- Tiagabine (Gabitril), Rufinamide (Banzel)
- Cannabidiol (Epidiolex): somnolence, sedation , for Lennox-Gastaut seizure.
Was this page helpful?
Back to top »