|
|
Pre-prandial |
Post-prandial |
|
Pre-diabetes |
100-125 |
140-199 |
|
Diabetes |
126 |
>200 |
|
Goal (ADA) |
80-130 |
<180 |
|
Goal (AACE) |
<110 |
<140 |
**A1C of 7% is 155mg/dL, with every 1% change in A1C is about 30mg/dL change in estimated average glucose level
5. Which of the following medications is contraindicated in a patient with heart failure?
1. D. Acarbose (Precose) is an oral alpha-glucosidase inhibitor. It delays the digestion of ingested carbohydrates, thereby resulting in a smaller rise in blood glucose levels following meals. Unlike sulfonylureas, Precose does not enhance insulin secretion. The recommended starting is 25 mg given orally three times daily at the start (with the first bite) of each meal. Hypoglycemia, gas, bloating and diarrhea are commonly reported side effects of Acarbose (Precose).
2. C. Canagliflozin - a sodium-glucose transporter (SGLT2), is the only option that decreases cardiovascular risk. Since this patient has nonvalvular atrial fibrillation and none of the other options decreases cardiovascular risk, empagliflozin is the most appropriate adjunct therapy to further lower this patient’s BG.
3.B. Insulin preparations should not be used if frozen or exposed to temperature > 98.6° F. Once opened, vials may be stored in the refrigerator or at room temperature, for up to 28 days.
4.C. Sitagliptin 50 mg PO daily is an appropriate agent to lower the A1c as needed and at an appropriate dose for renal function. Bydureon would be inappropriate due to the history of medullary thyroid carcinoma. Pioglitazone would not be a good choice due to its potential to decrease bone mineral density and given the patient’s weight of 190 lbs. Although insulin glargine would be an appropriate option, the dose of 30 units daily is too high as a starting dose.
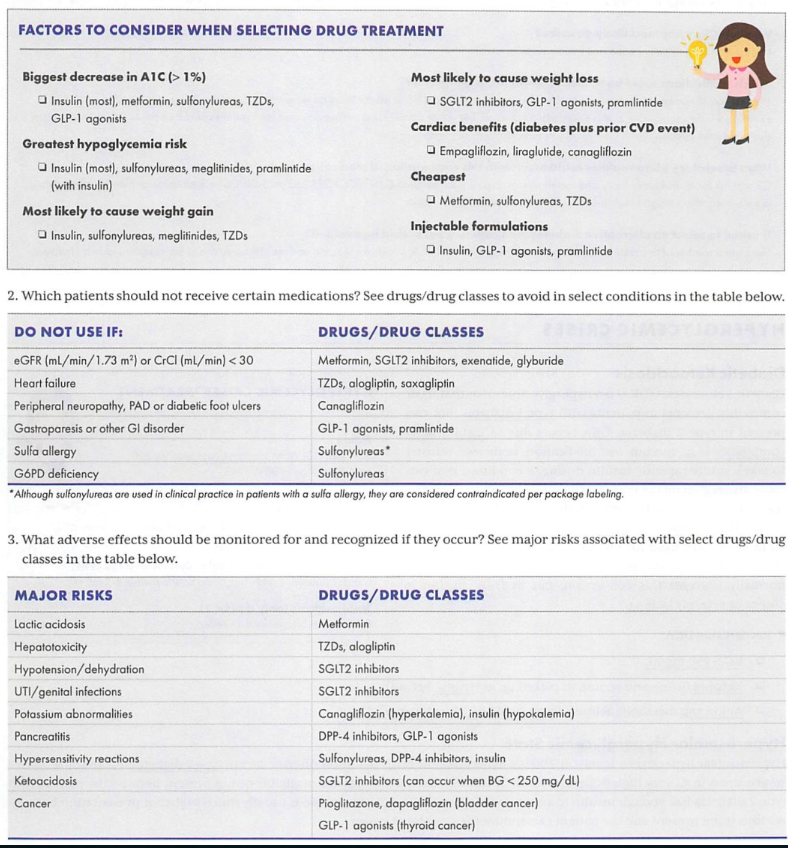
5.D. Pioglitazone is contraindicated in a patient with heart failure. Thiazolidinediones have a side effect profile that includes fluid retention/edema and has demonstrated increases in heart failure exacerbations. The class should be avoided in patients with heart failure, especially NYHA classes III and IV.
6.C. Sulfonylureas such as glyburide have the greatest risk of hypoglycemia among the listed agents. Metformin does not cause hypoglycemia as monotherapy. Although sitagliptin and liraglutide can cause hypoglycemia, the risk is significantly lower than with secretagogues.
7. B. Exenatide is a glucagon-like peptide agonist that, by mimicking this incretin hormone, results in glucose-dependent insulin secretion, slowed gastric emptying, and diminished glucagon secretion postprandially.
8.B. Metformin is contraindicated in patients with SrCr >1.4 for females. Pancreatitis is not a contraindication to the use of metformin. Decompensated heart failure is a contraindication to the medication, but this patient’s heart failure is currently compensated (NYHA class I).
9. A. Afrezza is a rapid-acting inhaled insulin that is administered at the beginning of each meal. Afrezza is not a substitute for long-acting insulin. Afrezza must be used in combination with long-acting insulin in patients with type 1 diabetes. It is not recommended for the treatment of diabetic ketoacidosis, or in patients who smoke. Afrezza has a BBW that acute bronchospasm has been observed in patients with asthma and COPD. Afrezza should be avoided in patients with chronic lung disease. The most common adverse reactions were hypoglycemia, cough, and throat pain or irritation.
10. BCE. Bydureon is a long-acting GLP-1 Agonist.
11: C. When using NPH and Regular insulin, the total daily dose is given 2/3 as NPH and 1/3 as Regular insulin. NPH is generally given BID and Regular insulin is given before meals. Type 1 Insulin Initiation: 0.6 units/kg/day = TDD; If using basal-bolus insulin, give ½ as basal and ½ as bolus.
12: A D E. NPH and Regular insulins do not require a prescription. Always wipe the injection site with an alcohol swab before administration.
13: E. [(blood glucose now) – (target blood glucose)]/(correction factor) = correction dose; Correction factor/dose: used to correct high BG.
14: B. When using basal and mealtime insulin (called a bolus) dosing strategy, it is initiated by giving 50% of the TTD as the basal dose and 50% as the bolus, or mealtime dose.
15: D. A1C of 7% = 154mg/dL, every 1% change in A1C is about 30mg/dL change in glucose.
16: ABE. Beta-blockers, particularly the non-selective, lipophilic agents can block shakiness, anxiety, and palpitations, but not sweating and hunger.
17: C. Metformin (Glucophage) is contraindicated with Scr ≥ 1.5 mg/dL (males) or ≥ 1.4 mg/dL (females). Metformin only needs to be stopped prior to the use of iodinated contrast dyes, but not contraindicated. Caution in heart failure, but not contraindicated unless they decompensated.
18: D. Humalog 75/25 contains 75% insulin lispro protamine and 25% insulin lispro. 25% of the 10 units = 2.5 units.
19: B C D E. Thiazolidinediones: PPARy-agonists, increase peripheral insulin sensitivity. Pioglitazone (Actos) – do not use in patients with bladder CA. SEs: peripheral edema, weight gain, edema, increase fracture risk.
20: A, B, D. According to JNC 8, initial therapy for diabetes should begin with an ACE inhibitor or angiotensin receptor blocker since the patient has chronic kidney disease. Thiazide-like diuretics and DHP CCBs are generally used for additional BP control in most patients.
Was this page helpful?