Last updated on: Jan 8th, 2020
Background
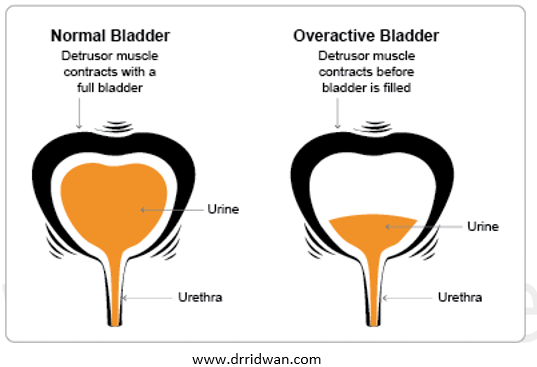
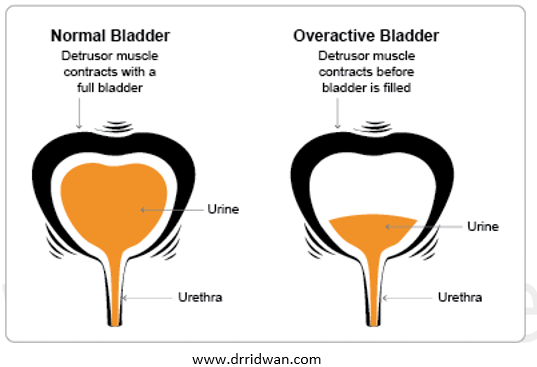
- Overactive bladder (OAB) is an inappropriate stimulation of muscarinic receptors on detrusor muscle causing frequent contractions and feeling or urgency before the bladder is full.
- OAB can lead to incontinence. Co-morbidities can exist include falls and fractures, skin infection, UTI, depression, sexual dysfunction. Classic symptoms: Urinary urgency, urinary frequency, nocturia.
- The detrusor muscle is mostly innervated by the parasympathetic nervous system (acetylcholine acting on muscarinic receptors), while the bladder neck is innervated by the sympathetic nervous system. Therefore, the mainstream of treatment for overactive bladder is anticholinergic agents.
- Muscarinic M2 and M3 receptors are located on bladder, M3 receptor is responsible for emptying contraction and involuntary contraction.
- BPH is the most common cause. Other risk factors: Age>40 yo, restricted mobility, obesity, vaginal delivery, hysterectomy, pelvic injury.
Forms of incontinence
- Functional: no abnormality, but patients may be socially, cognitively, physically impaired.
- Overflow: quantity of urine exceeds its capacity. E.g: benign prostate hyperplasia (BPH)
- Stress: leak during exertion (coughing, exercise, sneezing)
- Urge: cannot hold long enough, can be associated with neuropathy: DM (polyuria), stroke (damages neurons), dementia, Parkinson disease (movement disorder), Multiple sclerosis (disabling of CNS, affecting muscle functionality impact contractility of muscles controlling urine)
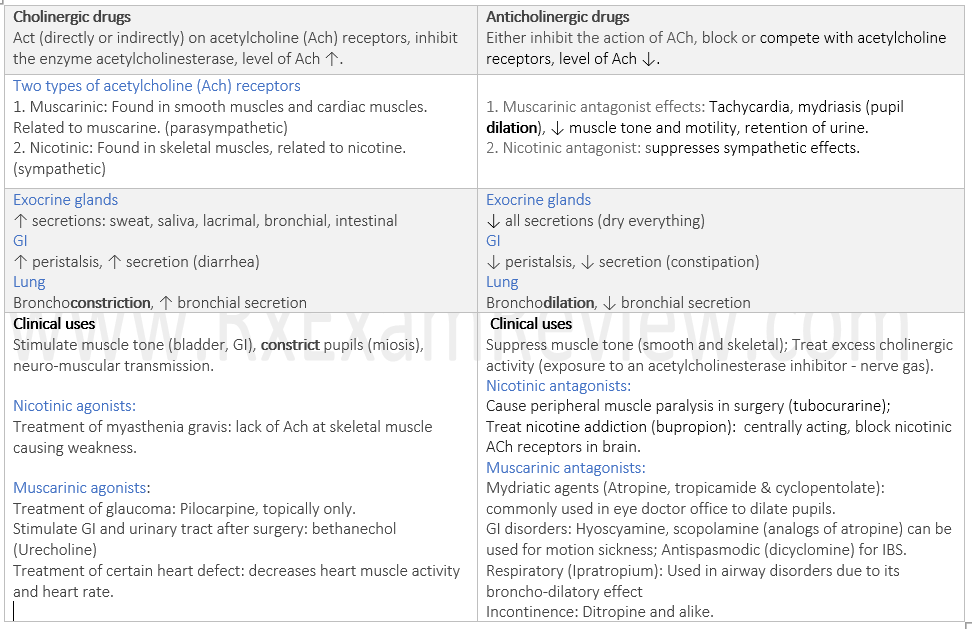
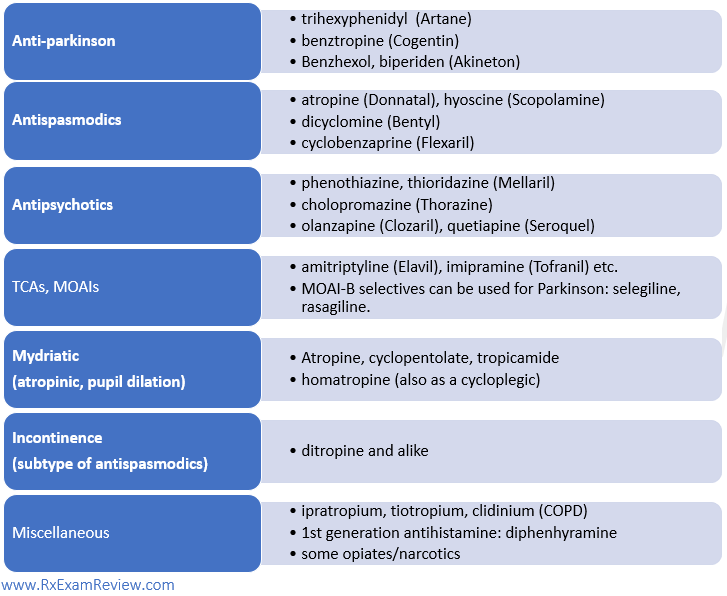
Anticholinergic drugs
- Drugs: Oxybutynin (Ditropan), Toterodine (Detrol), Trospium (Sanctura), Solifenacin (Vesicare), Darifenacin (Enablex), Fesoterodine (Toviaz).
- MOA: muscarinic receptor antagonist that competes with Ach receptor, block contraction of the detrusor muscle.
- CI: urinary retention, bladder obstruction, narrow angle glaucoma (cholinergic drugs have clinical use in treating glaucoma, inversely, anticholinergics do the opposite and worsen this acute type of glaucoma!)
- SE: GI: Constipation, paralytic ileus, urinary retention; Secretions: dry mouth/eyes, constipation; Eyes: blurred vision, mydriasis (pupil dilation); CNS effects: sedation, hallucination, cognitive impairment, delirium; Lungs: bronchodilation;
- Extended release is preferred over immediate release due to less drying effects (e.g: dry mouth).
- Drugs more selective for M3 receptors, have fewer CNS effects, than the older, non-selective agents oxybutynin.
- You should be very familiar in recognizing anticholinergic drugs and their effects, also remember they should be avoided as much as possible in elderly patients over 65 (Beers criteria recommendation), due to risk of delirium and cognitive impairment.
- If a question asks you on the appropriate treatment for a 65 y/o patient, eliminate the anticholinergic agents, and consider the co-morbidities.
- Can you list other anticholinergic agents? You should be able to identify antimuscarinic agents in treatment for peptic ulcer, parkinsonism, overactive bladder, motion sickness.
- Have a general idea about their dosing, doses listed here are recommended doses. Start low then increase the dose 1-2 weeks later to an optimal therapeutic level.
- Oxybutynin: 5 – 10mg QD. XL tab, patch (Oxytrol) and topical gel (Gelnique) causes less dry mouth; rotate site every day.
- Toterodine: 1 – 2mg BID; Trospium: 20mg BID; reduce dose in renal impairment <30.
- Darifenacin: 7.5 – 15mg QD, Solifenacin: 5 – 10mg QD, Fesoterodine: 4 – 8mg QD.
Beta-3 agonist
- Drug: mirabegron (Myrbetriq)
- MOA: causes relaxation of detrusor muscle by acting as beta-3 receptor agonist.
- SE: hypertension (opposite effect of beta blockers).
- Similar efficacy to anticholinergics and causes less dry mouth. Drug of choice in patients who cannot tolerate anticholinergics.
- DI: a moderate inhibitor of 2D6.
Botox (Onabotulumtoxin A)
- MOA: affect detrusor activity by inhibiting the release of acetylcholine.
- SE: urinary retention, dysuria, UTI.
- Third line option for patients who failed anticholinergics and mirabegron.
Nocturia
- Many causes: BPH, DM, overactive bladder, sleep apnea, heart failure, etc.
- Non-pharmacological: limit fluids intake before bed, limit salt, compression stocking and leg elevation.
- Treatment:
- loop diuretics (if QD, dose midafternoon, if BID, dose AM and midafternoon)
- desmopressin: caution on hyponatremia, on beers criteria in elderly.
- Desmopressin (DDAVP po inj., Noctiva nasal)
- MOA: an antidiuretic hormone analog that temporarily ↓ urine production.
- SE: hyponatremia (Na follows water).
- Boxed warning: hyponatremia and seizure.
- Avoid: renal impairment, severe hyponatremia (CKD, SIADH), fluid retention (HF, uncontrolled HTN), meds (diuretics, steroids, SSRIs, or chronic NSAIDs)
- Do not substitute Noctiva for other desmopressin nasal sprays, do not shake bottle, prime in first use, store in the fridge, dispense with MedGuide, 1 spray in either nostril before bed, for elderly cut dose in half, may increase to regular dose if Na+ level is normal
Was this page helpful?
Back to top »