Updates: July 27th, 2021
Oct 26th, 2020
July 14th, Apr 30th, 2020
Drug removal
- Majority is excreted through urine, and a small percentage through feces, other routes include lung, skin, tears and breast milk.
- Drugs and their metabolites need to be water soluable to be renally excreted.
- Many drugs are lipid soluble (non-polar, uncharged), and need to be converted to be water soluble (polar, charged).
CYP (Cytochrome) P450 enzymes
- One of the important functions of liver is detoxification. Cytochrome P450 will react with a whole bunch of substrates, because of that, there can be problems when we take medications. We can have a decrease in drug efficacy because P450 perceives these medications as toxins or foreign bodies, liver is going to try to detoxify them.
- Are essential for the metabolism of many medications. Although this class has more than 50 enzymes, six of them metabolize 90 percent of drugs, with the two most significant enzymes being CYP3A4 and CYP2D6.
- CYP enzymes are polymorphic (different forms of the same enzyme), changes are due to single nucleotide polymorphism (SNP) which can cause increase or decrease in drug metabolism rate. (ultra-rapid, extensive, intermediate, or poor metabolizer)
- Inducers: cause higher level of enzymes, metabolize drugs faster, leading to lowered level of drugs
- Inhibitors: inactivate enzymes leading to lower level of enzyme, metabolize drugs slower leading to increased levels of the substrate drugs.
- A strong inhibitor causes >5 times increase in plasma concentration; a moderate inhibitor causes >2 & <5 times increase.
Strong inducers: (↓ substrate drug level)
- Trick: instead of memorizing the full list using mnemonic, just memorize this shorter list of inducers and the rest would be inhibitors.
- phenytoin (Dilantin), phenobarbital (Luminal), oxcarbazepine (Trileptal)/eslicarbazepine (Aptiom), carbamazepine (Tegretol, also an auto-inducer): all AEDs except valproic acid (an inhibitor)
- Rifampin (and its derivatives)
- St. John’s Wort: the only herbal
- Smoking (1A2): lifestyle
- Some HIV drugs, for example most PIs are CYP inhibitors, some act as both inducer and inhibitor.
Strong inhibitors: (↑substrate drug level)
- Food: Grapefruit, alcohol (acts as a competitive inhibitor of Cp450, prevent it from metabolizing barbiturate, the patient did not feel the drowsiness effect of barb and took more, which lead to overdose of barb, and eventual death).
- Antimicrobials: azole antifungals, macrolides (clarithromycin, erythromycin, except azithromycin)
- Protease inhibitors, cyclosporine (Neoral/Sandimmune) | Cimetidine (Tagamet, H2RA agent, androgen-blocking effects (can cause gynecomastia - swollen, painful breast tissue or impotence)
- Amiodarone
- Non-DHP CCB’s [Diltiazem (Cardizem) | Verapamil (Calan)]
- Others: Statins (atorva/lova/simvastatin), pravastatin is a safer choice when drug interaction is a concern.
- Strong 1A2 inhibitors: fluvoxamine, ciprofloxacin, or enoxacin,
- Moderate/weak 1A2 inhibitors: oral contraceptives, estradiol, zafirlukast, zileuton, caffeine, acyclovir, Isoniazid
- 3A4 inhibitors: Amiodarone, azoles, cyclosporin, macrolides, non-DPHs, statins, PI
- 2D6 inhibitors: SSRIs (sertraline, escitalopram, paroxetine, fluoxetine)
- 2C19 inhibitors: cimetidine, esomeprazole, protease inhibitors, fluoxetine/fluvoxamine, azoles, modafinil, topiramate
- **Did you notice that strong inhibitors appear in a lot of places, it can be inhibitor of multiple enzymes?
Permeability glycoproteins (P-gp)
- MOA: Efflux transporters found in the gut and other organs, pumping drugs back out of bloodstream (into the gut).
- P-gp inhibitors: If a drug is subject to efflux and the transporter is inhibited by a different drug, the substrate drug concentration will increase.
- Common substrates: CV drugs (digoxin, carvedilol, ranolazine), anticoagulants (“-xabans” and dabigatran), calcineurin inhibitors (cyclosporine, tacrolimus/sirolimus), colchicine, some HCV drugs, ketoconazole, erythromycin, quinidine.
- Common inhibitors: anti-infectives (clarithromycin, some azoles), CV drugs (amiodarone, non-DHP CCBs, etc.), HIV (ritonavir, cobicistat) and HCV drugs, cyclosporine, ticagrelor.
Prodrug
- They are converted to the active form by the enzymes.
- Inhibitors will decrease the level of prodrug (drug cannot be converted properly to its active form), and inducers will increase the level of the prodrug. (This is opposite effect of the above)
- Common prodrugs: clopidogrel (2C19), tamoxifen (2D6), codeine (2D6).
Drugs with significant interactions
Amiodarone
- A moderator CYP inhibitor as well as a P-gp inhibitor, and a CYP enzyme substrate.
- Decrease dose 30-50% of these drugs when starting amiodarone: digoxin, warfarin, quinidine/procainamide (QT prolongation from increased level of anti-arrhythmics).
- Amiodarone ↑warfarin concentration (↑ risk of bleeding, amiodarone is a moderate CYP inhibitor) and ↑digoxin concentration (digoxin is a P-gp substrate).
- Use lower level of statins (simvastatin, lovastatin, atorvastatin), because statins are strong inhibitors and can raise amiodarone to a dangerous level.
- Electrolyte abnormalities (Na, Ca, Mg, K) must be corrected before initiating anti-arrhythmic therapy, or else the risk of arrhythmia will be increased.
Warfarin
- Racemic: S-isomer is 3-5 times more potent than R-isomer. S-isomer is 2C9 substrate.
- Tamoxifen is contraindicated with warfarin (ꝉ warfarin level).
- Interact with NSAIDS (not the selective agent celecoxib, causes vasoconstriction), antiplatelet (Plavix, Effient).
- Vitamin K ↓ INR (warfarin is a K antagonist), PPI may ↑ INR.
- SSRI + SNRI → Bleed Risk! All medications in these classes ↑ bleeding risk. The common issue is with anticoagulants or other drugs that prevent clotting.
- Herbals with ↑ bleeding risk (not through INR): ginkgo biloba, fish oil, garlic, vitamin E
Plavix
- Substrate of 2C19.
- Avoid 2C19 inhibitors: cimetidine/esomeprazole, protease inhibitors, fluoxetine/fluvoxamine, azoles, modafinil.
- g: A 35 y/o male on clopidogrel (Plavix®), is experiencing acid reflux and goes to a local pharmacy to buy an anti-acid medication. He decides that omeprazole (Prilosec®) would be a great option. He asks the pharmacist if this drug would be a good choice. As the pharmacist, would this be appropriate?
- Answer: No. First, clopidogrel is activated by the liver enzyme 2C19. Omeprazole is known to inhibit the same liver enzyme 2C19, and it would prevent the enzyme to work. If the enzyme cannot work, it cannot activate clopidogrel. If clopidogrel is not activated, it cannot prevent clots. The patient is at higher risk for clotting.
Digoxin
- Metabolized through renal clearance, and partially hepatic; we care about digoxin’s drug interactions because it is one of the narrow therapeutic window drugs (0.8-1.2).
- Requires dose adjustment in renal dysfunction, hold dose if ARF.
- Increased digoxin level by: hypokalemia (K < 3.5 mEq/ml) and drugs causing ↓K (thiazide/loops, certain progesterone birth controls -drosperinone), CYP inhibitors (macrolides, azoles, non-DHP, calcineurin inhibitors, amiodarone etc.).
- Decreased digoxin level by: Cholestyramine/colestipol (binder), metoclopramide (motility agents lead to less digoxin absorption).
Lithium
- 100% renally cleared, thus interacts with drugs affect renal clearance; we care about Li’s drug interactions because it is one of the narrow therapeutic window drugs , high level leads to toxicity (Level is related to Na).
- Increased level by: hyponatremia (↓Na due to ↓ salt intake/dehydration or drugs (ACEI/ARB/diuretics), NSAID (vasoconstriction at renal tubule leads to less Li excretion and ↑ serum concentration).
- Decreased level by: increased salt intake (high level of Na), caffeine, theophylline.
- Increased risk of 5-HT syndrome if taken with serotonergic drugs.
- Increase neurotoxicity (ataxia, tremors, nausea) with phenytoin/carbamazepine, non-DPH CCBs (class IV antiarrhythmic).
Non-DHP CCBs
- Avoid using with other drugs further lower HR: beta blockers, clonidine (alpha adrenergic agonist), digoxin, amiodarone.
MAOIs (monoamine oxidase inhibitor)
- Non-selective MAOIs cause more serotonin syndrome (5HT) and hypertensive crisis (NE).
- Avoid use with tyramine rich food (↑ NE): aged cheese, air-dried meat, wines, beer, fermented, smoked.
- Avoid taking drugs that further ↑ epinephrine, NE, or DA: MAOIs also block reuptake of a bunch of neurotransmitters.
- MAOI -B are selective for DA (rasagiline, selegiline), are used in Parkinson: selegiline become non-selective at higher dose.
- Avoid use with other serotonergic agents: refer to depression chapter for a complete list of serotonergic agents, basically any drug that targets 5HT (SSRI/SNRI/TCA, mirtazapine, buspirone, Li, St. John’s wort, dextromethorphan, linezolid, muscle relaxants, triptans, etc.).
- 2 weeks wash-out period changing between serotonergic drugs (except 5 weeks switching from fluoxetine to an MAOI).
NSAIDs
- All cause edema, raise BP (including selective agents), thus increase CV risks.
- Non-selective ↑GI bleeding risk, COX2 selective (celecoxib) ↑ CV risk.
- May cause renal toxicity due to vasoconstriction in renal vessels, avoid in renal diseases.
- Do not use with lithium, because vasoconstriction can lower Li metabolism, leads to Li toxicity, and causes renal toxicity.
- Risk of cardiovascular toxicity (edema, BP effects), the risk is higher in COX-2 selective, except ASA (CV beneficial).
Oral contraceptives
- Decreased level and reduced efficacy by: antibiotics (increase OC metabolism: ampicillins, griseofulvin, TCN, sulfonamides), and CYP inducers (rifampin: backup method for 1.5 months, anticonvulsants, St John's wort, smoking).
Statins
- Risk of muscle toxicity: rhabdomyolysis, (muscle breakdown, lab CPK is used to asscess muscle injury), breakdown byproducts can accumulate in kidney and cause renal failure.
- Atorvas/lovas/simvastatin: increased risk of muscle damage with 3A4 inhibitors (either reduce their dose, or switch to pravastatin)
- Normally pravastatin is the choice of drug in DI issues (less CYP interaction, however it can still undergo P-gp metabolism), cyclosporine (P-gp inhibitor) can ↑ pravas/pitavastatin levels.
- Use with niacin increase muscle risk and liver toxicity, but Niaspan can be used with lower dose of simvas/lovastatin if needed.
- Increased muscle risk with gemfibrozil, fenofibrates is a safer combination.
Tamoxifen
- Tamoxifen is a prodrug and needs to be activated by enzyme 2D6 to be effective. Do not use with 2D6 inhibitors, they prevent conversion of tamoxifen to active metabolite, leading to ↓ level of tamoxifen and reduced efficacy.
TCN & quinolones
- Chelate with cations (Al/Mg/Ca/ Zn/ Iron, phosphate binders, multivitamins, dairy products), sucralfate (adhesive barrier for duodenal ulcer), result in ↓ drug absorption, require at least 2 hours separation.
Azole antifungals
- Strong 3A4 inhibitors.
- Voriconazole (Vfend) is notorious for drug interactions, it is also a substrate of several CYP 450 enzymes, the level can be dangerously high when given with drugs that inhibit its metabolism, or even with small dose increase!
Theophylline
- Metabolized by 1A2, 3A4, follow Michaelis-Menten saturable kinetics (A small increase in dose can lead to large increase in theophylline concentration). A lot of drugs follow this kinetics have narrow therapeutic window (e.g: phenytoin)
- Inhibitors ↑ theophylline level
- 1A2: OC, zafirlukast, zileuton, acyclovir, cimetidine, cipro, estradiol, fluvoxamine, Isoniazid
- 3A4: Amiodarone, azoles, cyclosporine, macrolides, non-DPH CCBs, statins, protease inhibitors.
- Theophylline will ↓ Li (due to increased renal excretion of Li, theophylline has similar effect to caffeine which acts as a diuretic), and ↓ zafirlukast.
Valproic acid (VPA) + lamotrigine
- VPA is an enzyme inhibitor, it inhibits lamotrigine metabolism. Increase risk of severe rash, titrate slowly. These drugs are rarely given together. If the two drugs are to be given together, a Lamictal Starter Kit is required to ensure proper use.
Oxycodone
- Increased opioid level with 3A4 inhibitors: respiratory depression, this is dangerous, suggest to keep a naloxone kit at home.
- Decreased level with 3A4 inducers, reduced pain management.
PDE5 inhibitors
- sildenafil, tadalafil, vardenafil are used in ED.
- 3A4 substrate subjection to inhibitor and inducers.
- Caution with drugs that lead to severe hypotension (e.g: nitrates), and non-selective alpha blockers (more orthostasis/dizziness; start low and titrate slowly); less with selective ones like tamsulosin because the effect is limited to the particular areas.
Colchicine
- Avoid P-gp, 3A4 inhibitors, especially in renal/hepatic impairment.
How to memorize side effects
- It’s best to take class-wide approach than focusing on individual drugs. For example: all NRTIs can cause both lactic acidosis and hepatic steatosis via mitochondrial toxicity. Some individual drugs in the class may have a higher likelihood of lactic acidosis, but the risks exist for the entire class.
- Find ways to incorporate what you’ve studied into your life. For example: you took a Benadryl pill for insomnia, it is a 1st generation antihistamine, but since it not only works on blocking H1 receptors, it also blocks some acetylcholine receptors centrally hence can lead to drowsiness, and drying effect.
- Group drugs together that can cause a certain reaction, e.g.:
- prolong QT interval: FQs, macrolides, antipsychotics, 5-HT3 antagonists, class Ia and III antiarrhythmics, etc..
- drugs that can cause hyperkalemia: RAAS inhibitors (ACEIs/ARBs/aliskren), K-sparing diuretics, heparin, SMT/TMP, etc..
- drugs that can cause hypokalemia: thiazide/loop diuretics.
- Synergistic drug-drug interactions
- 5HT syndrome: mood medicines (SSRI/SNRI/TCA, buspirone, mirtazapine, Li), stimulants (dextromethorphan, ephedrine and analogs such as pseudoephedrine), muscle relaxants (cyclobenzaprine), triptans/ergos, St John's wort, linezolid, some pain reliver (meperidine, tramadol).
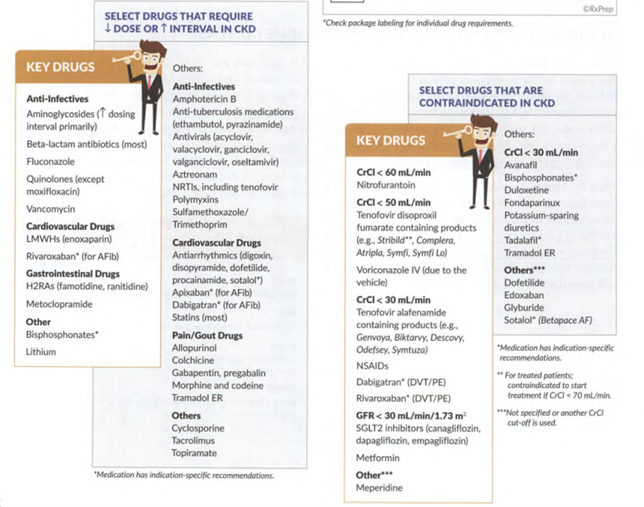
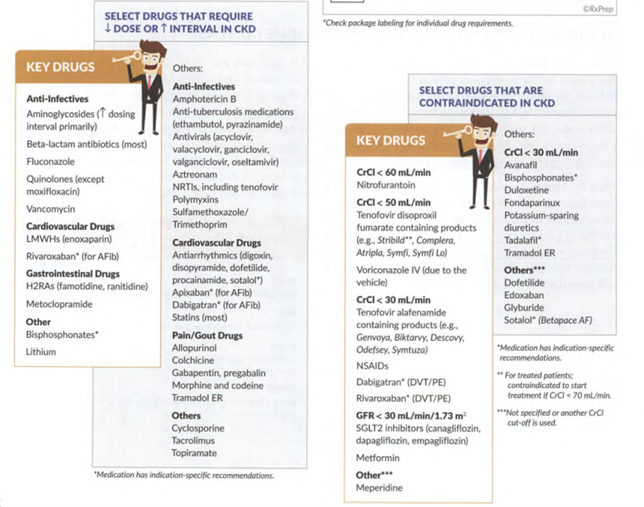
- memorize the exceptions to a rule. It would be impractical to memorize the massive list of every drug that requires a renal adjustment. An example here is the renal dosing of antibiotics. There are only a handful of commonly used antibiotics that don't require a renal adjustment.
- Abacavir is the only NRTI that does not require a renal adjustment.
- Ethambutol is the only drug in the RIPE regimen for TB that does not cause liver damage, so everybody else does.
- Captopril is the only ACE inhibitor dosed 3 times daily (and the only one that can be used in hypertensive urgency) for this reason we don’t usually see this drug a lot in retail dispensing.
- Most likely to cause immune reaction (hypersensitivity, rashes, allergy): PCNs, monoclonal antibodies, sulfa drugs, taxanes.
- Test for human leukocyte antigen (HLA), e.g: abacavir (HLA-B*5701) and carbamazepine (HLA-B*1502) have a very high risk of an immune reaction if given to individuals positive for the specific HLA.
Adverse drug reactions
- Med guides: required for original prescription and each refill. Not necessary to dispense to inpatients because they are being monitored. E.g: anticonvulsants, antidepressants, long-acting opioids, NSAIDS, ADHD and Strattera.
- Reporting: side effects, adverse events and allergies should be reported to FDA’s MedWatch program (FAERS), vaccines are reported under a different program VAERS.
- Phase IV: post-marking safety surveillance program.
- Mild rash: opioids cause a non-allergic release of histamine from mast cells, causing itches and hives.
- Photosensitivity: diuretics, quinolones, sulfa antibiotics, TCN, retinoids, amiodarone, methotrexate, etc.
- Thrombotic thrombocytopenic purpura (TTP: clots throughout the body): clopidogrel, ticlopidine.
- PCN and sulfonamides: two classes that cause the most drug allergies, each pharmacy has two separate counting trays for them.
- Sulfa allergy
- Sulfamethoxazole, sulfasalazine, sulfadiazine, sulfonamides/acetazolamide, thiazide and loop diuretics, sulfonylurea, zonisamide, celecoxib. Most contains “sulfa” or “amide”.
- Sulfate or sulfite (common preservative) do not cross react with sulfonamides, ok to take if someone has sulfa allergy.
- Biologics: Common to cause hypersensitivity reactions.
- Drugs to avoid in peanuts and soy allergy
- They belong to the same family and can cross react.
- clevidipine (Cleviprex), propofol (Diprivan), progresterone (Prometrium) capsules.
- Drugs to avoid in egg allergy: clevidipine (Cleviprex), propofol (Diprivan), yellow fever vaccine.
CNS depression
- Lipophilic drugs can enter CNS and cause sedation/confusion/impaired cognitive function.
- Alcohol, opioids, muscle relaxants, benzodiazepines, barbiturates, hypnotics, mirtazapine/trazodone, propranolol, clonidine, dronabinol/nabilone (treat loss of appetite in people with AIDS, as well as severe nausea and vomiting caused by chemo).
Hyperkalemia risk
- Renal disease: K is renally cleared.
- Increase K+ level: RAAS inhibitors, K-sparing agents, salt substitutes (KCl, lower risk for hypertension, but K replaces Na), oral contraceptive (newer generation such as Yasmin/Yaz contain drospirenone ↑K and clotting risk).
- May decrease digoxin level (renally cleared), hypo-K increases digoxin toxicity.
Treatment of hyper-K
- Discontinue any oral and IV potassium additives
- Give Ca2+ if K+ is critically high and EKG changes present (IV Ca gluconate or CaCl2), to stabilize cardiomyocyte membranes.
- Correcting K level has been a popular topic in NAPLEX.
Drive K intracellularly
- IV Insulin (plus dextrose to balance glucose level): 1st line therapy.
- β-2 agonist (e.g: albuterol solution) can be given STAT. Both β-2 agonist and insulin increase Na/K/ATPase pump activity, which drives K into cells.
- Sodium bicarb (HCO3-) to increase serum pH, the body will compensate to acidify itself to reach homeostasis phase by increasing H+/K+, HCO3-/K+ exchange (spits out protons to increase acidity and sucks K+ into the cell)
Remove K from body
- K-binder: sodium polystyrene sulfonate (Kayexalate) administered orally or rectally.
- Loop diuretic: side effect is significant hypokalemia. (Review notes from hypertension, loops excrete more K than thiazides)
Bleeding risk
- Anticoagulants: warfarin, heparin/LWMH, dabigatran, “-xabans”, agatroban/bivalirudin.
- Anti-platelets: salicylates (aspirin, dipyridamole), clopidogrel/prasugrel/ticagrelor
- SSRIs, SNRIs
- NSAIDs
- Natural products: ginkgo biloba/ginseng/garlic/ginger, fish oil, vitamin E
- PPIs can raise INR if patients on warfarin
QT prolongation
- QT interval measures how long it takes the heart to re-polarize (recharge) after each beat. In QT prolongation, the QT interval is abnormally prolonged, leaving the patient vulnerable to arrhythmias, especially torsade de pointes (symptoms: syncope, cardiac arrest). The risk depends on the dose and duration.
- Use following drugs with caution in existing cardiac conditions:
- Class Ia, III antiarrhythmics
- Antidepressants: TCAs, some SSRI/SNRI
- Antipsychotics: haloperidol, thioridazine, ziprasidone.
- Antibiotics: Quinolones and Macrolides.
- Azole antifungals.
- Antiemetics: 5HT3 antagonists, droperidol, phenothiazines antipsychotics (chlorpromazine, thioridazine, pimozide, etc.)
- Others: methadone, fingolimod, pentamidine (HIV infection-PCP)
Cholinergic Vs. anticholinergic drugs
Acetylcholine (Ach): is a common neurotransmitter released at neuromuscular junction and binds to receptors on muscle cells. In skeletal muscles, it leads to depolarization of cell membrane and causes muscle contraction (sympathetic), and an excitatory effect on visceral smooth muscle of the intestine (parasympathetic). However, it has an inhibitory effect on the heart (↓HR). Parasympathetic = “rest and digest”, sympathetic = “flight or flight”.
- Two types of acetylcholine receptors:
- Muscarinic: Found in smooth muscles and cardiac muscles, related to muscarine.
- Nicotinic: Found in skeletal muscles, related to nicotine.
Cholinergic
- MOA: Act (directly or indirectly) on Ach receptors, inhibit the enzyme acetylcholinesterase, level of Ach ↑.
- Effects on the body: Exocrine glands: ↑ secretions: sweat, saliva, lacrimal, bronchial, intestinal; GI: ↑ peristalsis, ↑ secretion (diarrhea); Lung: bronchoconstriction; pupils (constriction: miosis); Stimulate muscle tone (bladder, GI); Heart: ↓ heart rate (different Ach receptors located on the heart compared to smooth/skeletal muscles).S
- Clinical uses:
- Nicotinic agonists: Treatment of myasthenia gravis (flaccid muscle tone): Raise Ach at skeletal muscle to stimulate muscle tone.
- Muscarinic agonists: Treatment of glaucoma (miotic agent such as pilocarpine eyedrops, review vision disorder chapter), certain heart defect (decreases heart muscle activity and heart rate); Stimulate GI and urinary tract after surgery: bethanechol (Urecholine).
Anticholinergic
- MOA: Either inhibit the action of ACh, or block/compete with acetylcholine receptors, level of Ach ↓.
- Effects on the body: Exocrine glands:↓ secretions (dry everything: membrane, mouth, constipation); GI: ↓ peristalsis, ↓ secretion (constipation); Lung: Bronchodilation; Eye: pupil dilation (mydriasis); Suppress muscle tone (smooth and skeletal) and motility; Heart: ↑ heart rate (difference Ach receptors located on the heart compared to smooth/skeletal muscles).
- Clinical uses:
- Treat excess cholinergic activity (e.g: exposure to nerve gas: an acetylcholinesterase inhibitor).
- Nicotinic antagonists: suppresses sympathetic effects; cause peripheral muscle paralysis in surgery (tubocurarine); Treat nicotine addiction (bupropion): centrally acting, block nicotinic ACh receptors in brain.
- Muscarinic antagonists: GI disorders: hyoscyamine, scopolamine (analogs of atropine) can be used for motion sickness (recall anticholinergic effects on reduced motility); Antispasmodic (dicyclomine) for irritable bowel syndrome (again stopping the movement and drying effect); Incontinence: ditropine and alike (due to their drying effect and suppress muscle tone lead to retention of urine; Review chapter on “Overactive bladder”); Respiratory (anticholinergic inhalants: Ipratropium): due to its broncho-dilatory effect; Mydriatic agents (Atropine and alike): used in eye doctor office to dilate pupils;
- Many drugs are anticholinergics:
- Anti-Parkinson: trihexyphenidyl (Artane), benztropine (Cogentin), benzhexol, biperiden
- Antispasmodic: atropine (Donnatal), hyoscine (Scopolamine), dicyclomine (Bentyl), cyclobenzaprine (Flexeril)
- Antipsychotics: phenothiazine, thioridazine, chlorpromazine (Thorazine), olanzapine (Clozaril), quetiapine (Seroquel)
- TCAs, MOAIs: amitriptyline (Elavil), imipramine (Tofranil) etc.; MOAI-B selective can be used for Parkinson: selegiline, rasagiline.
- Mydriatic (atropinic) eyedrops: Atropine, cyclopentolate, tropicamide, homatropine (also as a cycloplegic).
- Incontinence (subtype of antispasmodic): ditropine and alike.
- Anticholinergics used in COPD: ipratropium, tiotropium, clidinium.
- 1st generation antihistamine: diphenhydramine, meclizine (Antivert)
- Some opiates/narcotics.
Phenylketonurics (PKU)
- PKU: A genetic disorder, inability to metabolize phenylalanine because of a lack of the enzyme phenylalanine hydroxylase.
- Phenylalanine is precursor of tyrosines (NE, DA, epinephrine).
- Presentation of this disease state is mental retardation, notice the above neurotransmitters (NE &DA), play huge roles in mental disorders.
- Individuals with this disorder must avoid intake of phenylalanine.
Avoid alcohol
- Disulfiram(Antabuse): acts as an enzyme inhibitor (acetaldehyde dehydrogenase), preventing the metabolism of acetaldehyde into acetic acid, and is used in the treatment of alcoholism.
- A disulfiram-like drugcan cause hypersensitivity to alcohol (N/V, flushing, dizziness, throbbing headache, chest and abdominal discomfort, and general hangover-like symptoms), these effects are caused by accumulation of acetaldehyde - a toxic metabolite of alcohol.
- Many disulfiram-like drugs act as inhibitors of acetaldehyde dehydrogenase similarly to disulfiram. Many of them are antibiotics, patients take these medications should avoid alcohol.
- Cephalosporins(cefamandole, cefmenoxime, cefmetazole, cefonicid, cefoperazone, cefotetan, ceftriaxone, cefuroxime, and latamoxef (moxalactam))
- Metronidazole, sulfonamides, sulfonylurea.
- Other meds to avoid taking with alcohol: Oral corticosteroid/NSAIDs (GI upset), phenytoin/BZDs (act centrally, the toxicity resembles alcohol overuse).
Discoloration (urine or feces)
- Instead of rote memorization, view discoloration as a drug property being very hydrophilic that it stains the fluids.
- Iron, phenazopyridine (Azo).
- Cefdinir, Nitrofurantoin.
- Rifampin, Rifapentine: a rifamycin derivative for treatment of TB.
Hepatotoxicity risk
- Drugs that are lipophilic or drugs that are part of CYP metabolism likely carry hepatotoxicity.
- TB meds (Rifampin, isoniazid)
- APAP overdose, alcoholism
- Antifungal drugs (ketoconazole, terbinafine)
- Anticonvulsants (phenytoin, phenobarbital)
- Rheumatoid arthritis drugs: such as infliximab (Remicade), chloroquine, hydroxychloroquine.
Nephrotoxicity risk
- Drugs that are hydrophilic and mostly renally cleared are more likely to be nephrotoxic.
- Platinum-based chemo (cisplatin), rheumatoid arthritis drugs: such as infliximab (Remicade), chloroquine, hydroxychloroquine.
- Vancomycin, aminoglycoside, amphotericin B: renal toxicity is significant.
- NSAID (including COX2 inhibitors): vasoconstriction in renal vessels.
- Loop diuretics: volume depletion, inadequate renal perfusion, and making kidney work hard.
- ACEI/ARB: renal protective however can also be damaging in bilateral renal stenosis (efferent tubules are already stiff and can no longer distend and dilate).
- Calcineurin inhibitors (CNIs): cyclosporin, tacrolimus.
- Li, digoxin: 90-100% renal clearance!
Ototoxic Agents
- These drugs are known to cause hearing toxicities. A trivia here is that drugs that cause renal toxicities to great extent usually cause ototoxicity (the outer ear resembles shape of kidney).
- Vancomycin, aminoglycosides, loop diuretics (especially IV), salicylates (Magnesium salicylate (Doan Pills), ASA: tinnitus (ringing in the ear), platinum-based chemo.
Antidotes
|
APAP
|
N-acetylcysteine (NAC, Acetadote, Mucomyst in CF)
|
|
Anticoagulants (warfarin)
|
Phytonadione (Mephyton)
|
|
Anticholinesterase insecticides (nerve agent), cholinergic symptoms
|
Atropine/pralidoxime (Protopam), anticholinergic properties
|
|
Anticholinergic
|
Physostigmine (Antilirium): a cholinergic agent
|
|
Arsenic, lead
|
Succimer (Chemet)
|
|
Benzos
|
Flumazenil (Romazicon): treat drowsiness from sedative procedure, also used off-label for hypnotic overdose (Ambien)
|
|
Beta blockers
|
Glucagon
|
|
Botulism
|
Botulism antitoxin
|
|
CCB
|
Calcium chloride 10%, glucagon
|
|
Carbon monoxide
|
Oxygen
|
|
Cyanide
|
Cyanokit (Sodium nitrate, sodium thiosulfate): dark red color
|
|
Digoxin
|
Digoxin immune fab (Digibind, DigiFab)
|
|
Ethylene glycol, methanol
|
Ethanol or fomepizole
|
|
Heavy metals
|
Dimercaprol/penicillamine
|
|
Heparin
|
Protamine
|
|
Iron
|
Deferoxamine (Desferal)
|
|
Isoniazid
|
Pyridoxine (V-B6)
|
|
Methemoglobinemia
|
Methylene blue
|
|
Opioids
|
Naloxone (Narcan, Evzio)
|
|
Salicylate - ASA, TCA
|
Sodium bicarbonate: increase pH of urine results in ASA elimination
|
|
Snake bites
|
Crotalidae polyvalent (Antivein)
|
|
Alcoholics
|
V-B1, reduce neurotoxicity, protect nerve system
|
|
hyperammonemia from valproic acid (valproate).
|
L-carnitine
|
Quiz
- A 70-year-old female (5′ 3″, 80 kg) has a stable serum creatinine of 1.5 mg/dL. Which is an accurate assessment of her renal function?
- Stage 1 CKD
- Stage 2 CKD
- Stage 3 CKD
- Stage 4 CKD
- A 60-year-old man (5′ 10″ , 92 kg) presents for annual follow-up. He has a medical history of hypertension. 2 months ago, his BP was 145/95 mmHg, serum creatinine was 1.6 mg/dL, and urine albumin:creatinine = 10 mcg:mg. Values today include: BP 145/95 mmHg, HR 84, K = 4.5 mEq/L, SCr= 1.5 mg/dL, and urine albumin:creatinine = 10 mcg:mg. Which of the following is the best recommendation?
- Chlorthalidone
- Lisinopril
- Amlodipine
- Non-pharmacological therapy only
- A female patient with stage 3A CKD and HTN presents at follow-up with a BP reading at last visit = 136/86. She began non-pharmacological therapy at that time. Vital signs today include BP 136/84 and HR 88. Labs: K = 4.2 mEq/L, SCr = 1.4 mg/dL, and urine albumin:creatinine = 100 mg:g. Which would be the best recommendation?
- Initiate chlorthalidone
- Initiate lisinopril
- Initiate amlodipine
- Non-pharmacological therapy only
- Which of the following is the most appropriate therapy in a patient with stage 4 CKD and edema?
- Indapamide
- Spironolactone
- Bumetanide
- HCTZ
- A patient with stage 3 CKD presents for a routine follow-up and has the following lab results: vitamin D 40 ng/mL, PTH 115 pg/mL, phosphate 5.3 mg/dL, Ca 9.9 mg/dL, albumin 3 mg/dL. Which is the most appropriate therapy to start at this time?
- Renagel
- Calcitriol
- Ca acetate
- Ergocalciferol
Answers
- D. Calculated via Cockcroft-Gault equation, patient’s estimated creatinine clearance = 29 mL/min. Stage 4 CKD’s estimated GFR (calculated CrCl) is15– 29 mL/min.
- A. This patient’ s estimated GFR = 52 mL/min placing him into stage 3 CKD (45– 59 mL/min). His urine protein <30 mcg:mg, patients with non-proteinuric BP goal is <140/90 and thus pharmacotherapy is indicated. 1st line therapy is thiazide-type diuretic (such as chlorthalidone). An ACEI would be first-line if he had proteinuria.
- B. Patient has CKD with proteinuria (>30), her BP goal is <130/80 mmHg. First line therapy for patients with CKD and proteinuria is an ACEI or ARB. Thiazide diuretics are first line in a patient with non-proteinuric CKD.
- C. Patients with stage 4 CKD have an estimated GFR <30 mL/min, which requires loop diuretics (or metolazone), whereas thiazide diuretics would be ineffective. Additionally, loop diuretics are more effective in treating edema as compared to aldosterone antagonists and thiazide diuretics.
- A. This patient has complications of CKD: hyperphosphatemia and hyperparathyroidism. Both sevelamer (Renagel) and calcium acetate (Phoslo) are phosphate binders. Calcium containing phosphate binders, should be avoided in hyper-Ca and the patient’ s vitamin D level is at goal (>30).
Was this page helpful?
Back to top »